Pharmacy Education: Learn Medication Safety, Drug Interactions, and Patient Care
When you think about pharmacy education, the training and knowledge base that prepares pharmacists and patients to use medications safely and effectively. Also known as medication safety training, it’s not just about counting pills—it’s about understanding why a drug works, who it might hurt, and how culture, age, or other meds can change everything. Most people assume pharmacists just fill prescriptions, but real pharmacy education teaches how to spot a deadly drug combo before it’s too late, how gut bacteria can turn a harmless pill into a poison, and why someone might refuse a generic just because it’s the wrong color.
This isn’t theory. It’s daily reality. A 72-year-old on five meds might not know one of them raises their risk of falling. Someone with a penicillin allergy might actually just had a stomach ache. And in some cultures, patients won’t take a generic because they believe the white pill isn’t as strong as the blue one. medication safety, the practice of preventing harm from drugs through proper use, monitoring, and communication means catching these gaps before someone ends up in the ER. It’s why the FDA tracks side effects long after a drug is approved, why labs are needed on a schedule for certain meds, and why doctors now use checklists based on real-world data like the Beers Criteria to avoid dangerous combinations in older adults.
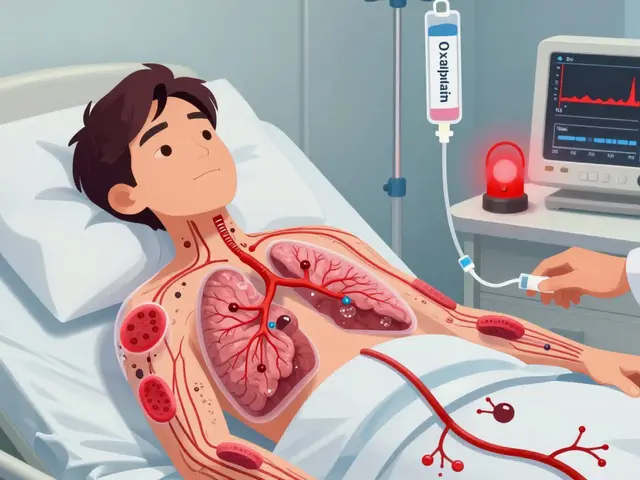
Real drug interactions, when two or more medications affect each other’s effects or safety, often leading to unexpected side effects or reduced effectiveness don’t always show up in textbooks. They show up when a statin and a new heart drug cause muscle damage, or when a sleep aid and an antibiotic combine to slow breathing to dangerous levels. patient adherence, how consistently a person takes their medication as prescribed, often influenced by side effects, cost, or cultural beliefs isn’t just about remembering to take your pill—it’s about trust, cost, and even the shape of the tablet. And generic medications, lower-cost versions of brand-name drugs with the same active ingredient, but often misunderstood due to appearance, branding, or misinformation aren’t just cheaper—they’re everywhere, and people’s beliefs about them can make or break treatment.
What you’ll find here isn’t a lecture. It’s the kind of stuff you wish you’d known before starting a new med. How to read a lab calendar to catch liver damage early. Why some cholesterol drugs work better together at low doses. How to tell if a reaction is a true allergy or just a side effect. What to watch for when traveling with meds. How kidney function changes with age—and why that changes your dose. These aren’t academic points. They’re life-saving details buried in plain sight.

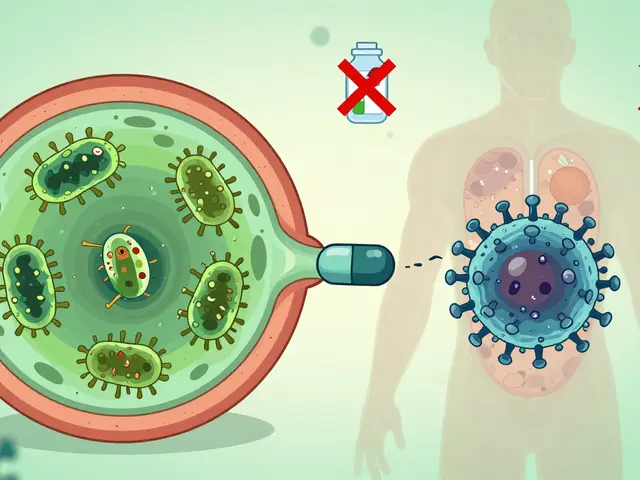
Health Literacy and Generics: Closing the Knowledge Gap That Costs Lives
Many people stop taking their medication because they don't understand that generics are just as effective as brand-name drugs. Closing this knowledge gap saves lives, reduces hospital visits, and cuts healthcare costs.
view more