
Medication Heat Risk Calculator
This tool helps you assess your risk of heat-related illness based on medications and other factors. Understanding your risk can help you take appropriate precautions during hot weather.
Your Heat Risk Assessment
When temperatures climb, people taking certain blood‑pressure or bladder‑control pills face a hidden danger: their meds can turn a hot day into a health emergency. Understanding why diuretics and anticholinergic drugs make you more heat‑vulnerable, and what you can do about it, saves lives.
What the drugs do - and why heat matters
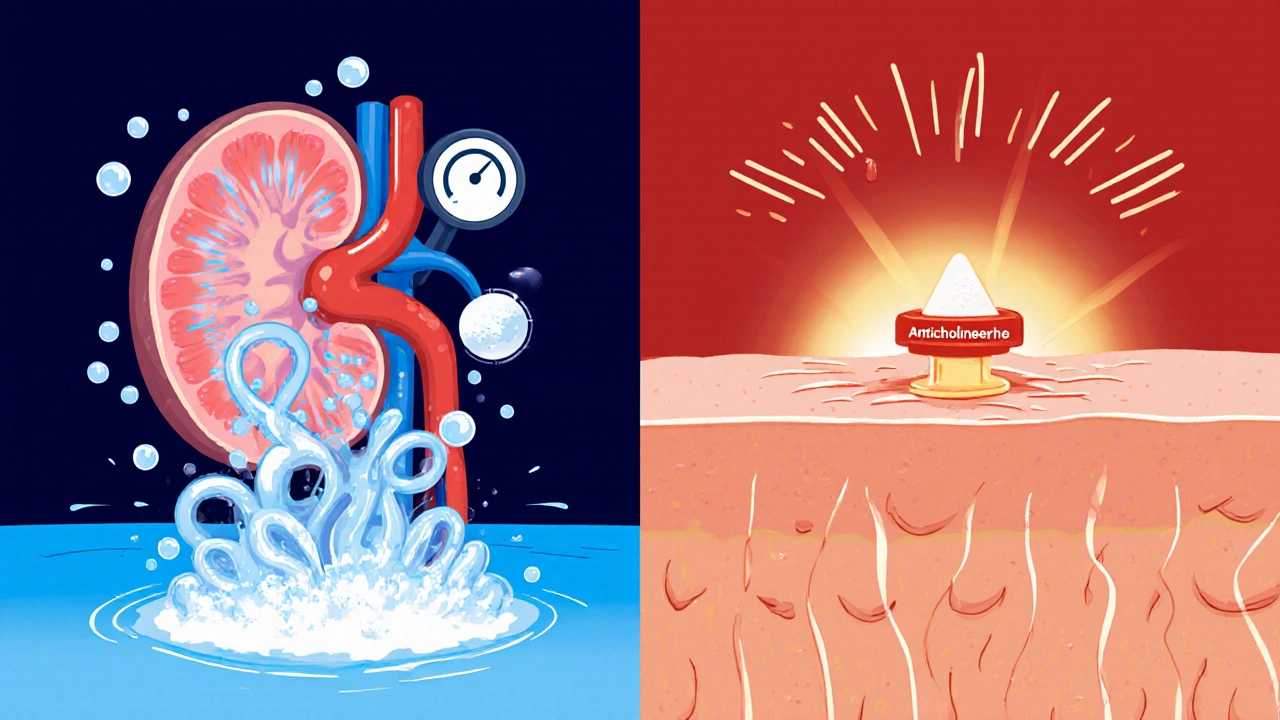
Diuretics are a class of medicines that increase urine output to lower blood pressure or remove excess fluid in heart‑failure patients. Common examples include furosemide (Lasix) and hydrochlorothiazide (Microzide). By pushing sodium and water out of the body, they help the heart work easier, but they also shave away the fluid reserve you need to replace when you sweat.
Anticholinergic medications block the neurotransmitter acetylcholine at muscarinic receptors. Drugs such as oxybutynin (Ditropan) for overactive bladder and the antidepressant amitriptyline (Elavil) fall into this group. Their main side‑effect in hot weather is the suppression of sweating - the body’s natural cooling system.
The Centers for Disease Control and Prevention (CDC) flags both classes as high‑risk during heat events because they each attack a different part of thermoregulation.
How diuretics raise the stakes
When you’re in a heat wave, you can lose 1-2 liters of fluid per hour just by sweating. Loop diuretics like furosemide stop the kidney’s thick ascending limb from re‑absorbing sodium, which means you can’t concentrate urine and hold onto water. Thiazide diuretics add potassium loss, leading to hypokalemia that can impair the heart’s rhythm under stress.
Research published in the Journal of Thermal Biology (2023) showed that participants on strong anticholinergic‑burden drugs (ACB = 3) had blunted core‑temperature responses; the same pattern appears for diuretics, but the data are scarcer. A 2022 national study of Medicare beneficiaries found loop‑diuretic users were 37 % more likely to be hospitalized for heat‑related illness than non‑users, even when temperatures stayed below 80 °F (26.7 °C).
How anticholinergics block your cooling system
Sweat glands need acetylcholine to fire. Anticholinergics bind to muscarinic receptors and shut that signal down. The result: a 30-50 % drop in sweat production for drugs with an anticholinergic burden score of 3. Without sweat, your skin can’t evaporate heat, and core temperature climbs faster.
During the 2021 Pacific Northwest heat dome, 91 % of the 800+ heat‑related deaths involved at least one medication that interfered with thermoregulation, and diuretics or anticholinergics were present in 63 % of those cases.
Heat exposure precautions you can start today
- Hydration strategy: Aim for 2-3 L of water a day if you’re on a diuretic, unless your doctor has set a stricter fluid limit for heart‑failure management. Sip frequently; don’t wait until you feel thirsty.
- Electrolyte check: A simple at‑home potassium test strip can alert you to low levels that increase cardiac risk.
- Medication review: Talk to your prescriber about temporary dose reductions during prolonged heat waves. Some clinics used a protocol in July 2022 that cut furosemide by 25 % for 5 days, reducing dehydration without compromising blood‑pressure control.
- Environment control: Stay in air‑conditioned spaces between 68-72 °F (20-22 °C). If you must be outside, seek shade, wear a wide‑brimmed hat, and choose lightweight, light‑colored clothing.
- Buddy system: Have a friend or family member call twice a day during heat alerts. Anticholinergic users may develop confusion that masks early heat‑illness signs.
- Sunscreen: Apply broad‑spectrum SPF 30+; many anticholinergics increase photosensitivity, raising burn risk.
Quick checklist for clinicians
| Aspect | Diuretics | Anticholinergics |
|---|---|---|
| Primary thermoregulation impact | Fluid loss & electrolyte imbalance | Sweat suppression |
| Key warning signs | Dizziness, dry mouth, dark urine | Overheating, dry skin, confusion |
| Suggested dose tweak | Temporary 20‑30 % reduction in extreme heat (under supervision) | Consider switching to lower‑burden agent or tapering |
| Monitoring frequency | Weight & urine output daily | Temperature & mental status twice daily |
Emerging research and future directions
The National Institute on Aging has earmarked $4.2 million for studies focusing on medication‑heat interactions in older adults. Early results suggest that combining a loop diuretic with a high‑burden anticholinergic multiplies risk more than either alone.
Dr. W. Larry Kenney’s NIH‑funded project at Penn State (R01AG077821) is testing heat tolerance in people over 60 who take common diuretics or anticholinergics. Preliminary data due this summer show a 15 % faster rise in core temperature for participants on both drug classes.
Meanwhile, the CDC’s Heat and Health Tracking System is integrating prescription‑fill data to create real‑time risk maps. In the next few years, clinicians may receive alerts like, “High‑risk patient on furosemide within 30 mi of 95°F forecast - consider outreach.”
Bottom line
Diuretics and anticholinergic medications each chip away at the body’s ability to stay cool. By adjusting fluids, watching electrolytes, reviewing doses, and staying connected with a support person, you can blunt the heat‑related danger. Keep an eye on the evolving research - the science is catching up, but the practical steps are already solid.
Should I stop my diuretic during a heat wave?
Never stop it on your own. Talk to your doctor; they may lower the dose temporarily or adjust the timing, but an abrupt stop can spike blood pressure or cause fluid overload.
How much water is safe if I have a fluid restriction for heart failure?
During extreme heat, many clinicians advise a modest increase -‑ for example, adding 500 ml to your usual limit, but only after confirming your weight and kidney function.
Can over‑the‑counter antihistamines increase heat risk?
Yes, many first‑generation antihistamines have anticholinergic properties (ACB = 3). If you’re already on a prescription anticholinergic, adding one can further cut sweating.
What early symptoms should trigger a call to emergency services?
Rapid heartbeat, confusion, dizziness, nausea, or a body temperature above 104 °F (40 °C) require immediate medical attention. Heat stroke can develop quickly in medication‑vulnerable patients.
Are there safer alternatives to high‑burden anticholinergics?
For overactive bladder, mirabegron (a beta‑3 agonist) carries little anticholinergic load. For depression, newer SSRIs lack the sweating‑block effect. Discuss switches with your prescriber.






12 Comments
Wow, this post really dives deep into the pharmaco‑thermoregulation nexus, and as a fellow bio‑engineer I can appreciate the mechanistic jargon they dropped. The interplay between loop diuretics and the renal Na‑K‑2Cl cotransporter is a classic case of iatrogenic hypovolemia. On top of that, anticholinergics hit the muscarinic receptors on eccrine glands – that’s why sweat production plummets. Folks on furosemide should especially watch their serum electrolytes and weigh themselves daily, otherwise they risk orthostatic hypotension. Bottom line: stay hydrated, monitor labs, and keep your doc in the loop. Its crucial to act before the heat hits.
Thanks for breaking down the risks so clearly – staying on top of fluid intake and checking potassium levels can truly be life‑saving. I’ll make sure to discuss dose adjustments with my cardiologist before the next heat wave.
These meds make you melt in the heat, lol 😂
Man, I never thought my water pills could turn a sunny day into a nightmare. The body’s cooling system is like a fragile balloon, and these drugs just let the air out. If you’re out in the sun, you’re basically cooking on low‑heat. So keep that AC on and sip water like it’s your job.
Imagine your body as a finely tuned orchestra, each organ playing its part. When diuretics or anticholinergics steal the rhythm, the whole symphony can go off‑key, especially under a scorching sun. But with mindful hydration, electrolyte balance, and a touch of sunshine mindfulness, you can keep the music alive 🌞. Think of each sip of water as a note of harmony, each doctor’s advice as a conductor’s cue.
Indeed, the clinical evidence, as highlighted in the Journal of Thermal Biology, suggests a statistically significant increase, 37 % higher, in heat‑related hospitalizations among loop‑diuretic users; furthermore, the anticholinergic burden, quantified as ACB = 3, correlates with a 30‑50 % reduction in sweat output; consequently, patient education becomes paramount, and providers must tailor dosage regimens accordingly.
Dear community, I commend the thoroughness of this exposition and wish to emphasize the importance of proactive communication with healthcare professionals; a collaborative approach ensures that fluid restrictions are judiciously managed while preserving cardiovascular stability 😊. Additionally, incorporating regular temperature monitoring can preempt adverse events.
When evaluating the thermoregulatory challenges posed by diuretics and anticholinergics, it is essential to adopt a multidimensional perspective that encompasses physiology, pharmacology, and environmental factors. First, the kidneys’ role in conserving sodium and water becomes compromised under the influence of loop diuretics, leading to a net negative fluid balance that diminishes plasma volume. Second, plasma volume contraction reduces cardiac output, which in turn impairs heat dissipation through peripheral circulation. Third, anticholinergic agents interfere directly with the cholinergic pathways that activate eccrine sweat glands, effectively silencing one of the body’s primary cooling mechanisms. Fourth, the synergistic effect of simultaneous diuretic and anticholinergic therapy can precipitate a rapid rise in core temperature, as documented in recent cohort studies. Fifth, electrolyte disturbances, particularly hypokalemia and hyponatremia, predispose patients to cardiac arrhythmias when exposed to thermal stress. Sixth, older adults often exhibit blunted thirst perception, making self‑regulated hydration less reliable. Seventh, the prevalence of polypharmacy in this demographic amplifies the risk of drug‑drug interactions that may further compromise thermoregulation. Eighth, public health data from the 2021 Pacific Northwest heat dome illustrate that a majority of heat‑related fatalities involved at least one thermoregulatory‑impairing medication. Ninth, clinicians can mitigate these risks by implementing temporary dose reductions, scheduling medication administration during cooler periods of the day, and encouraging patients to maintain a daily fluid log. Tenth, point‑of‑care potassium testing kits provide a pragmatic method for monitoring electrolyte status without requiring laboratory visits. Eleventh, community outreach programs that deliver cooling centers and hydration stations can serve as vital safety nets for high‑risk individuals. Twelfth, technological advances such as wearable temperature sensors paired with electronic health record alerts hold promise for real‑time risk stratification. Thirteenth, ongoing NIH‑funded trials are exploring pharmacogenomic markers that may predict susceptibility to heat‑related adverse events. Fourteenth, policymakers should consider integrating prescription‑fill data into heat‑alert systems to facilitate targeted interventions. Fifteenth, patient education materials must be culturally sensitive and linguistically accessible to ensure broad adoption. Finally, while the scientific community continues to unravel the complex interplay between medication and heat stress, the practical steps outlined herein remain readily actionable and can substantially reduce morbidity and mortality.
It is ethically unacceptable to prescribe high‑burden anticholinergics without counseling patients on heat‑risk mitigation; physicians must uphold their duty of care.
Our great nation shouldn't let bureaucratic med‑prescriptions turn its citizens into walking ovens! 🇺🇸 When the sun beats down, we need bold policies that protect the health of patriots, not lax guidelines that let pharma dominate. Adjust doses, fund cooling shelters, and demand accountability from drug companies now! 🔥💪
Great tips stay cool and safe stay awesome
One could argue that heat is a metaphor for life's pressures and medication the veil that obscures our true resilience 😊; yet awareness and intentional action peel back that veil revealing the innate capacity to adapt