
Every year, millions of people in the U.S. stop taking their medicine-not because it doesn’t work, but because they don’t understand what they’re taking. And the biggest confusion? Generic medications.
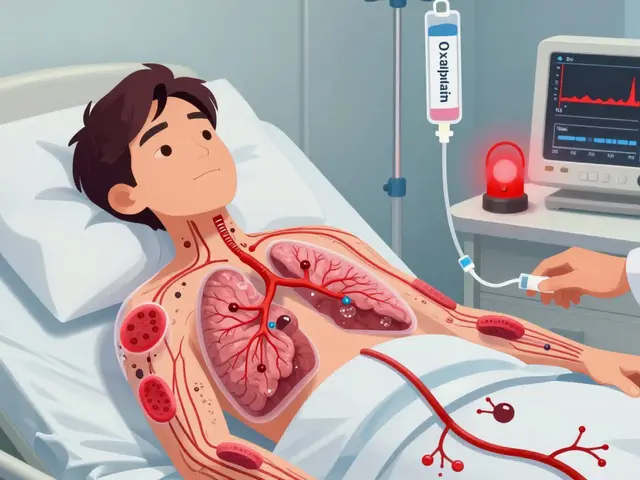
Picture this: You’ve been on a brand-name blood pressure pill for years. One day, your pharmacist hands you a different-looking tablet-smaller, white instead of blue, no logo. You’re told it’s the same drug. But you’re not sure. Is it weaker? Is it safe? You’ve heard stories. You’re scared. So you don’t take it. Or you take it inconsistently. And then you end up in the hospital.
This isn’t rare. It’s happening right now, in living rooms, in pharmacies, in clinics across the country. And it’s not about being careless. It’s about a gap in understanding that’s been ignored for too long.
What Health Literacy Really Means (And Why It Matters for Your Pills)
Health literacy isn’t just being able to read. It’s knowing what the words on your pill bottle mean. It’s understanding why your doctor switched your medication. It’s being able to ask the right questions when something doesn’t look familiar.
The U.S. government defines it as the ability to find, understand, and use health information to make smart choices. That includes reading labels, counting pills, knowing when to take them, and recognizing when a new-looking pill is actually the same drug you’ve been on for years.
Here’s the hard truth: Only 12% of U.S. adults have proficient health literacy. That means nearly nine out of ten people struggle with basic medical instructions. And when it comes to generics, the numbers get worse.
Studies show that 47% of people with low health literacy don’t realize generic drugs contain the exact same active ingredients as brand-name ones. That’s not a small misunderstanding. That’s a safety risk. People stop taking life-saving meds because they think the cheaper version is a knockoff.
Why Do Generics Look So Different?
Generics aren’t fake. They’re not cheap imitations. They’re FDA-approved copies. The law says they must work the same way, in the same amount, with the same strength and purity as the brand-name drug.
So why do they look different? Because the law only requires the active ingredient to match. The color, shape, size, and even the taste? Those are controlled by the manufacturer. They change them to avoid copying the brand’s trademarked appearance.
But patients don’t know that. They see a different pill and assume it’s a different drug. A 2023 survey found that 62% of negative reviews about generics were because of appearance. One patient on Reddit said they stopped their blood pressure medication because the generic looked like a "street drug." Another thought switching to a generic was being prescribed a new antidepressant-and almost overdosed.
It’s not their fault. No one explained it. No one showed them a side-by-side picture. No one said, "This is the same medicine, just in a different jacket."
The Cost of Not Knowing
When people don’t understand generics, they pay more. They skip doses. They go to the ER. They get hospitalized.
People with low health literacy are 32% more likely to be hospitalized because of medication mistakes. And 18% of those hospitalizations are directly tied to confusion over generics. That’s not just a health issue-it’s a financial one.
Generics make up 90% of all prescriptions filled in the U.S. But they cost only 23% of what brand-name drugs do. That’s billions in savings-money that could go to care, not wasted pills.
Yet, because patients don’t trust generics, they often demand the brand. Insurance plans pay more. Employers pay more. Patients pay more in co-pays. And the system pays more in emergency visits and complications.
One study found that when patients understood generics, they were 14% less likely to end up in the ER. That’s $675 saved per person every year. Multiply that by millions-and you’re talking about a $1.2 billion problem that could be fixed with better communication.
Who Gets Left Behind?
This isn’t a problem for everyone equally. The people most affected are the ones already struggling: elderly patients, immigrants, non-English speakers, people with lower incomes, and those with chronic illnesses.
Immigrants and limited English speakers are 3.2 times more likely to misunderstand generic medication info. Imagine being handed a prescription in a language you barely read, then being told the pill looks different now-and you’re supposed to trust it.
Older adults often have multiple prescriptions. A change in pill shape can trigger confusion with other meds. They may not remember what they’re taking, let alone why a new pill is okay.
And yet, only 38% of healthcare organizations have any kind of program to help patients understand generics. Most pharmacists spend just 4.2 minutes explaining a switch. For patients with low health literacy? That jumps to nearly 10 minutes. But most don’t get that extra time.
What Actually Works to Close the Gap
It’s not about more flyers. It’s not about yelling at patients to "read the label." It’s about communication that sticks.
One proven method? The Teach-Back technique. Instead of saying, "Do you understand?"-which most people say yes to, even if they don’t-pharmacists ask: "Can you tell me in your own words why you’re taking this pill?"
Studies show this cuts misunderstandings by 42%. Patients who go through Teach-Back are 83% more likely to stick with their meds.
Another fix? Visual aids. A simple side-by-side photo of the brand and generic pill, with the same active ingredient highlighted. A diagram showing that the blue pill and the white pill both contain "amlodipine." No jargon. Just pictures and plain words.
Some pharmacies now use apps that let patients scan their pill and see a photo, name, and explanation. One study found this improved recognition by 35%.
And the FDA? They launched a Generics Awareness Campaign in 2023. Plain language brochures. Videos. Training for pharmacists. It’s a start.

What You Can Do Right Now
If you’re taking any medication-brand or generic-ask yourself these questions:
- Do I know the name of the active ingredient in my pill?
- Have I ever been switched to a generic? Did someone explain why?
- If the pill looks different, do I know it’s still the same medicine?
- Can I explain my meds to someone else-like a family member or caregiver?
If you can’t answer those, ask your pharmacist. Don’t wait until you’re confused or scared. Ask before you run out.
Bring your pill bottle to the pharmacy. Point to the generic. Say: "Can you show me how this is the same as the one I was on?"
Don’t be embarrassed. You’re not alone. And you’re not stupid. You just never had the right information.
The Bigger Picture
This isn’t just about pills. It’s about trust in the system. People don’t mistrust generics because they’re irrational. They mistrust them because they’ve been left out of the conversation.
Healthcare systems spend millions on fancy apps and AI tools. But the simplest fix-clear, patient-centered explanations-is still rare.
Starting in 2024, Medicare Part D plans are required to assess health literacy. That’s a big step. But real change happens one conversation at a time.
When a pharmacist takes 10 extra minutes to show a patient a picture of two pills and say, "This is the same medicine. The only difference is the price,"-that’s not just education. That’s saving a life.
Generics aren’t second-best. They’re the smart choice-for your wallet, your health, and the system. But they only work if you understand them.
Knowledge isn’t power. Applied knowledge is. And right now, millions are missing out-not because they don’t care, but because no one told them how.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and stability. The only differences are in inactive ingredients (like color or filler) and cost. Generics are tested to ensure they work the same way in the body.
Why do generic pills look different from brand-name ones?
By law, generic manufacturers can’t copy the exact appearance of brand-name pills to avoid trademark issues. That’s why color, shape, size, or markings may differ. But the active ingredient-the part that treats your condition-is identical. A blue pill and a white pill can both contain the same medicine; the difference is just the coating or dye.
Can switching to a generic make my medication less effective?
No, not if it’s FDA-approved. Generics must be bioequivalent, meaning they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA allows a small range (80-125%) for absorption differences, but this is based on decades of research and applies to nearly all patients. For most people, switching to a generic has no effect on how well the drug works.
What should I do if I think my generic isn’t working?
Don’t stop taking it. Talk to your pharmacist or doctor first. Sometimes, side effects or changes in how you feel are due to inactive ingredients-not the active drug. For example, a different filler might cause mild stomach upset. Your provider can check if you’re taking the right dose, if another generic version might suit you better, or if you need to return to the brand. Never assume the generic is weaker.
How can I tell if my prescription was switched to a generic?
Check the label. Generic medications are clearly labeled with the generic name (like "amlodipine") and often include the manufacturer’s name. Your pharmacy receipt will also show if it’s a generic. If you’re unsure, ask the pharmacist: "Is this a generic version?" They’re required to tell you. Many also provide a handout explaining the switch.
Is it okay to switch between different generic brands?
Yes. Multiple companies make generics for the same drug, and they’re all FDA-approved. Switching between them is safe. However, if you notice a change in how you feel after switching generics (like new side effects), tell your provider. It’s usually due to inactive ingredients, not the active drug, but it’s worth checking.
Why don’t doctors explain generics better?
Many doctors assume patients understand, or they’re pressed for time. But the real issue is that health literacy isn’t taught in medical training. Doctors often don’t know how to explain it simply. That’s why pharmacists are often the best resource-they have more time and are trained in patient communication. If your doctor doesn’t explain, ask them to refer you to the pharmacist for a detailed review.
Are there tools or apps that help me understand my generic meds?
Yes. Apps like Medisafe, MyTherapy, and the FDA’s Pill Identifier let you scan or search your pill to see its name, active ingredient, and photos. Some pharmacies offer printed guides with side-by-side images of brand and generic versions. Ask your pharmacist if they have these. Visual tools improve understanding by up to 35% compared to verbal explanations alone.
If you’re managing a chronic condition, don’t let confusion about your meds hold you back. Knowledge is the cheapest, most powerful medicine you can take.


13 Comments
It’s wild how we treat medicine like it’s a magic trick-same ingredients, different packaging, and suddenly it’s ‘not the real thing.’ We’ve built a culture where trust is tied to branding, not science. A pill doesn’t care if it’s blue or white. It only cares if it’s in your system. The real crisis isn’t the generic-it’s our collective refusal to unlearn the myth that cost = quality.
It is absolutely imperative to recognize that the systemic failure in health literacy is not merely an educational deficiency-it is a structural pathology embedded within the very architecture of pharmaceutical distribution, regulatory oversight, and provider-patient communication paradigms. The FDA’s bioequivalence standards, while scientifically rigorous, are rendered functionally inert when patients are not provided with multimodal, linguistically accessible, and culturally competent educational interventions that actively dismantle the cognitive dissonance induced by visual dissimilarity. Without mandatory visual comparison tools, standardized pharmacist-led Teach-Back protocols, and federally funded public awareness campaigns, we are merely rearranging deck chairs on the Titanic of medication nonadherence.
My grandma switched to generic blood pressure pills last year and she still takes them every day like clockwork. No drama. No confusion. Just her and her little white pill. The pharmacist showed her a picture on his phone. That’s all it took. People think it’s complicated but sometimes it’s just about showing up and saying hey this is the same thing
Oh wow so the system is just *designed* to make poor people feel stupid so they stop taking their meds? Shocking. The pharmaceutical companies don’t want you to know generics are identical because then they’d have to lower prices. And the doctors? They’re too busy scrolling through their phones to explain anything. This isn’t ignorance-it’s exploitation. And now we’re supposed to be grateful for a 35% improvement from scanning apps? Please. We need a revolution. Not a pamphlet.
Let me be clear: this entire issue stems from a fundamental lack of personal responsibility. If you cannot comprehend a prescription label, it is not the fault of the healthcare system-it is your failure to prioritize your own well-being. The FDA does not hand out hand-holding services. You are not entitled to a visual aid. You are entitled to a pill. Take it. Or don’t. But do not blame the pharmacist for your inability to read. And please stop using emoticons when discussing life-or-death medical decisions. It’s unprofessional.
Man in Nigeria we face this every day but worse-no one even tells you it’s generic. You just get a new pill and you’re like ‘what is this poison?’ But we adapt. We ask neighbors. We call relatives abroad. We don’t wait for a brochure. We don’t wait for a fancy app. We just figure it out. America thinks it’s a crisis because you have too much time to be scared. We don’t have that luxury. We take the pill. Period.
The bioequivalence range of 80–125% is statistically sound, but the psychological impact of visual change is not accounted for in clinical trials. There’s a cognitive dissonance between pharmacokinetic equivalence and perceptual identity. The brain doesn’t process ‘same active ingredient’ as ‘same drug’-it processes color, shape, size. We need neurocognitive studies on pill perception, not just adherence metrics. The solution isn’t just education-it’s redesigning the user experience of medication.
I’ve seen this with my dad-he’s 72, on five meds, and he stopped one because the generic looked like a ‘street pill.’ He thought it was Xanax. I sat with him for an hour. We Google-searched both pills side by side. He cried. Not because he was scared-but because no one ever showed him how to check. That’s the tragedy. Not the pill. Not the cost. The silence. We need more people like my sister who just sits down and says ‘let’s figure this out together.’ That’s healthcare. Not apps. Not brochures. Presence.
My pharmacist gave me a little card with pictures of my brand and generic side by side. I stuck it on my fridge. I still have it. I don’t need to remember anything. I just look. It’s so simple. Why isn’t this standard? Why do we make people memorize medical jargon when a photo solves it? Also lol at people who think generics are fake. You’d think we were talking about counterfeit sneakers not lifesaving medicine
It’s not about the pill. It’s about being seen. When someone takes the time to say ‘I know this looks different, and that’s scary-but here’s why it’s safe’-that’s the moment trust is rebuilt. Not with a pamphlet. Not with an app. With a human voice. I’ve been on generics for years. I never had to ask. But I know so many who do. We need more of those quiet moments in pharmacies.
It’s fascinating how deeply we anthropomorphize medication-assigning personality to color, shape, and brand. We treat pills like they have identity, dignity, even loyalty. And yet, chemically, they’re inert molecules. The emotional weight we place on the physical form of a drug is a cultural artifact, not a medical one. Perhaps the real solution lies not in educating patients about generics, but in retraining ourselves to see medicine as a process-not a product with a logo.
People who don’t understand generics shouldn’t be allowed to take them. It’s that simple. You don’t get to be scared and then blame the system. If you can’t read a label, get help. Or don’t take it. But don’t make everyone else pay for your ignorance.
Let me tell you something they don’t want you to know: The FDA doesn’t test generics the same way as brand names. The ‘bioequivalence’ studies? They’re done on healthy volunteers-not the elderly, not diabetics, not people with liver disease. The real difference? It’s in the fillers. And those fillers? They’re not just inert. They’re linked to inflammation, gut issues, even depression. They’re hiding it. You think you’re saving money? You’re being experimented on. And they call it ‘generic’ to make you feel better about it.