HFrEF: Understanding Heart Failure with Reduced Ejection Fraction and How Medications Help
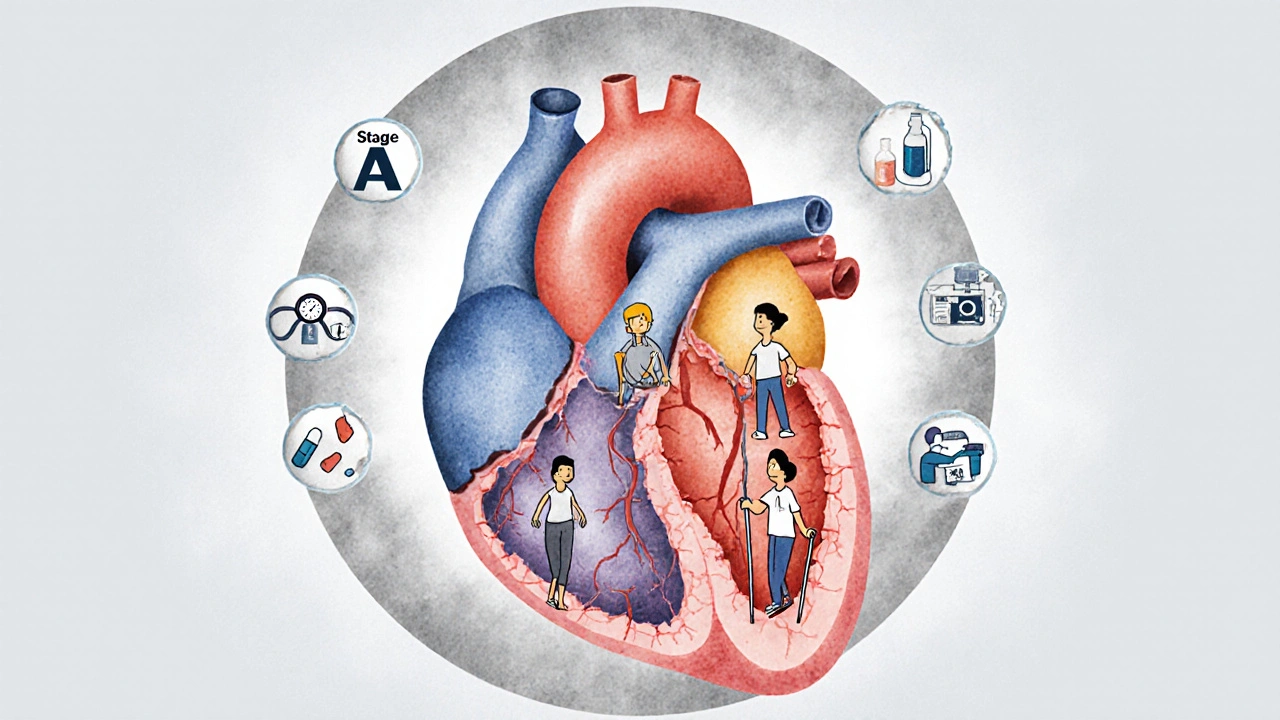
When your heart can’t pump hard enough to push blood through your body, it’s called HFrEF, a type of heart failure where the left ventricle doesn’t contract properly, leading to low ejection fraction. Also known as systolic heart failure, it’s not just about feeling tired—it’s about your heart’s ability to do its job. HFrEF means your heart’s ejection fraction (EF) is below 40%. That’s the percentage of blood pumped out with each beat. A healthy heart pushes out 55-70%. When it drops below 40%, your organs don’t get enough oxygen, and your body starts to break down.
What causes this? Often, it’s years of high blood pressure, past heart attacks, or diabetes damaging the heart muscle. But here’s the thing: HFrEF doesn’t just happen overnight. It creeps in. And the drugs you take for other conditions—like beta-blockers, diuretics, or even some diabetes meds—can make it worse if not monitored. That’s why Toprol XL (metoprolol), a beta-blocker used to slow heart rate and reduce strain on the heart is often part of the treatment plan. It’s not a cure, but it helps your heart work less hard. Same with Rybelsus (semaglutide), a GLP-1 drug originally for diabetes that’s now shown to reduce heart failure hospitalizations. Even if you don’t have diabetes, it might still help your heart.
HFrEF is closely tied to left ventricular failure, when the main pumping chamber of the heart weakens and can’t keep up. That’s why diabetes is such a big risk—it damages blood vessels and nerves that control your heart. And if you’re older or have kidney problems, your body can’t clear meds the way it used to. That’s why medication dosing, especially for drugs like digoxin or ACE inhibitors, must be adjusted based on kidney function. Too much? You risk confusion, falls, or even poisoning. Too little? Your heart keeps struggling.
What you’ll find in these articles isn’t theory—it’s real-world guidance. People share how they tracked side effects with lab calendars, switched from outdated HIV drugs that damaged their hearts, or found safer alternatives to nerve meds that made them overheated. Others detail how gut bacteria can turn a heart pill into a toxin, or why a penicillin label might be wrong and lead to worse choices down the line. These aren’t just drug reviews—they’re survival guides for living with a weakened heart.
You won’t find fluff here. Just straight talk on what works, what doesn’t, and what you need to ask your doctor before the next prescription. Whether you’re managing HFrEF yourself or helping someone who is, the tools, warnings, and comparisons below are built to help you stay out of the hospital—and keep your heart beating as long and strong as possible.
Heart Failure Management: From Diagnosis to Living Well
Heart failure management has changed dramatically. With new drugs like SGLT2 inhibitors and advanced monitoring tools, patients are living longer and better than ever. Learn how diagnosis, treatment, and daily care have evolved.
view more




