When your kidneys start to fail, your body doesn’t just slow down-it starts to swell. Edema in chronic kidney disease (CKD) isn’t just a nuisance; it’s a warning sign that your body is holding onto too much fluid. And if left unchecked, it can lead to high blood pressure, heart strain, and even hospitalization. The good news? You don’t have to just live with it. A clear, practical approach combining diuretics, salt restriction, and compression therapy can make a real difference in how you feel day to day.
Why Edema Happens in CKD
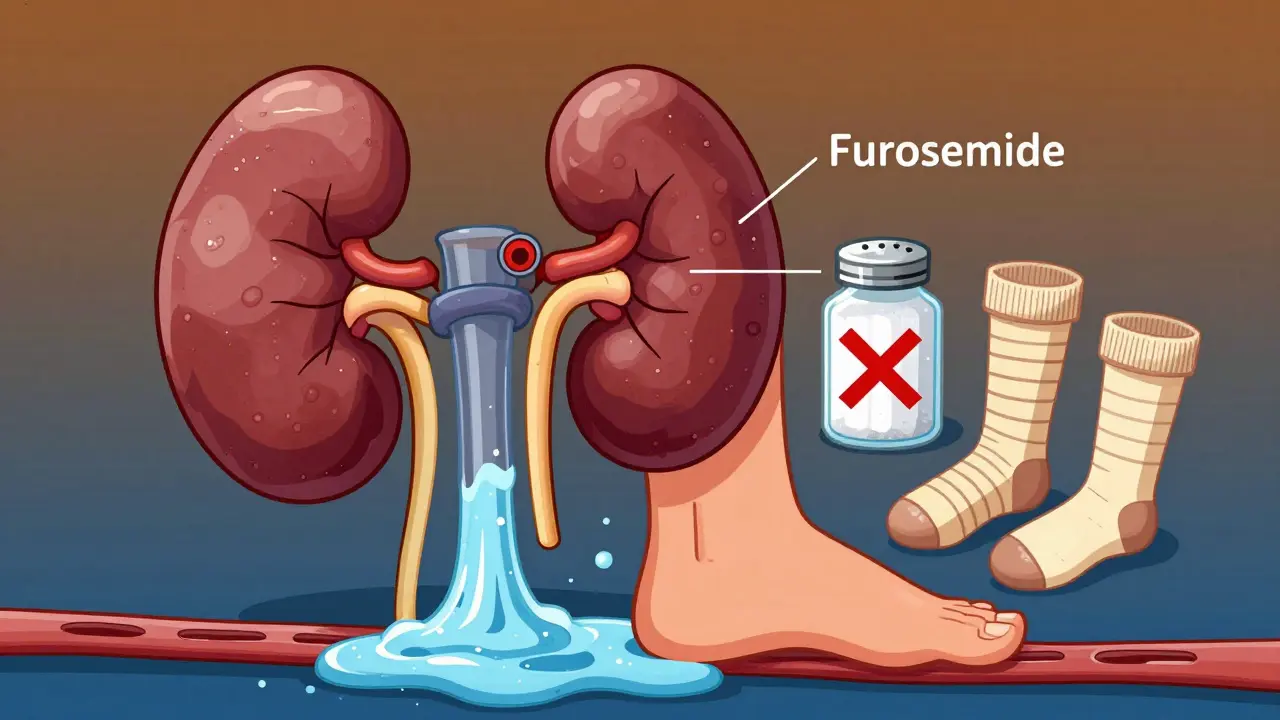
Your kidneys are like filters. They remove extra water and salt from your blood and send it out as urine. But when kidney function drops-especially in stages 3 to 5 of CKD-those filters start to clog. Sodium builds up in your bloodstream, and water follows it like a tide. That extra fluid doesn’t just stay in your veins; it leaks out into your tissues. That’s edema.
You’ll notice it first in your ankles and feet. Later, it might show up around your eyes in the morning, or make your belly feel tight and swollen. In advanced cases, fluid can even collect in your lungs, making it hard to breathe. This isn’t just about comfort-it’s about survival. Studies show that people with persistent edema have a 28% higher risk of dying from heart or kidney complications than those who manage their fluid balance well.
Diuretics: The Right Drug, at the Right Dose
Diuretics are often the first line of defense. But not all diuretics work the same, and not everyone needs them the same way.
If your eGFR is below 30 mL/min/1.73m² (that’s stage 4 or 5 CKD), loop diuretics like furosemide, bumetanide, or torsemide are the go-to. They work hard on the loop of Henle, the part of the kidney that reabsorbs the most salt. A typical starting dose is 40-80 mg of furosemide once a day. If that doesn’t do enough, doctors may increase it by 20-40 mg every few days-up to 320 mg daily in severe cases.
But here’s the catch: diuretics aren’t magic. A 2016 NIH study tracked 312 non-dialysis CKD patients and found that those on diuretics lost kidney function 3.2 mL/min/1.73m² per year, compared to just 1.7 mL for those not on them. That’s a faster decline. Why? Because diuretics can drop your blood pressure too low, reduce blood flow to the kidneys, and trigger acute kidney injury.
That’s why combination therapy matters. For patients with eGFR above 30, adding a thiazide like hydrochlorothiazide (12.5-25 mg daily) to a loop diuretic can boost fluid removal. This “sequential nephron blockade” works because it hits two different parts of the kidney. But it also increases the risk of kidney injury by 23% if not monitored closely.
Then there’s spironolactone. It’s not a typical diuretic-it blocks aldosterone, a hormone that makes you hold onto salt. It’s especially helpful if you also have heart failure (NYHA class III or IV) or severe ascites. But in late-stage CKD, it can spike potassium levels. Over 25% of patients with stage 4 or 5 CKD on spironolactone develop dangerous hyperkalemia. That’s why regular blood tests are non-negotiable.
And now, there’s a new tool: injectable furosemide. Approved by the FDA in March 2025, it’s designed specifically for patients with eGFR under 15. In trials, it cleared 38% more fluid than oral versions. For someone who can’t absorb pills due to gut swelling or nausea, this could be life-changing.
Salt Restriction: The Most Powerful Tool You Already Own
Here’s the truth: no diuretic works as well if you’re still eating too much salt. And most people have no idea how much they’re really consuming.
The National Kidney Foundation says you should aim for no more than 2,000 mg of sodium per day. For advanced CKD, go lower-1,500 mg. That’s less than a teaspoon of table salt. But here’s the kicker: 75% of your sodium doesn’t come from the salt shaker. It’s hidden.
Bread? Two slices = 300-400 mg. Canned soup? One cup = 800-1,200 mg. Deli meat? Two ounces = 500-700 mg. Even yogurt and fruits like watermelon carry sodium and fluid you might not think about.
Studies show that sticking to a 2,000 mg limit can cut edema by 30-40% in early-stage CKD-without any medication. But it’s not easy. A 2024 survey by the American Kidney Fund found that 68% of patients struggle with salt restriction. Why? Taste, social meals, and lack of access to low-sodium options.
Real success comes from education. Working with a renal dietitian for 3-4 sessions makes a huge difference. They teach you how to read labels, swap out processed foods, cook with herbs instead of salt, and spot hidden sodium in sauces, condiments, and frozen meals. And don’t forget fluids: limit total intake to 1,500-2,000 mL per day. That includes soups, yogurt, even ice cubes.

Compression Therapy: More Than Just Socks
When your legs swell, elevation helps-but only if you’re sitting still. Movement matters. That’s where compression therapy comes in.
Graduated compression stockings (30-40 mmHg at the ankle) are the gold standard. They squeeze your legs tighter at the bottom and looser at the top, helping blood and fluid flow back toward your heart. A 2022 study using water displacement volumetry found that wearing them daily for four weeks reduced leg volume by 15-20%.
But here’s the problem: only 38% of people keep wearing them after three months. Why? They’re hard to put on, cause skin irritation, or just feel uncomfortable. That’s why pairing them with movement is key. Walking 30 minutes a day, five days a week, improves lymphatic drainage and cuts edema by 22% compared to just resting.
For severe cases-like nephrotic syndrome or massive swelling-intermittent pneumatic compression devices can help. These machines inflate and deflate sleeves around your legs, mimicking muscle contractions. One 2020 study found they reduced leg circumference 35% more than regular stockings.
And don’t forget simple habits: elevate your legs above heart level for 20 minutes a few times a day. Sit in a chair with your feet on a stool. Lie down with pillows under your calves. These small changes add up.
The Real Challenge: Adherence and Risk
Managing edema in CKD isn’t about one magic solution. It’s about balancing three things: removing fluid, avoiding harm, and staying consistent.
Diuretics can help-but they can also hurt your kidneys if overused. Salt restriction works-but most people can’t stick to it. Compression helps-but it’s uncomfortable.
And then there’s the human side. A 2023 NHS survey found 78% of diuretic users said frequent urination ruined their sleep. 42% got muscle cramps. 35% felt dizzy. One in five had a fall or fainting spell from low blood pressure.
Successful cases? They all had the same thing: a team. A nephrologist to guide meds, a dietitian to teach food choices, and a physical therapist to help with movement and compression. One Mayo Clinic registry showed that with this team approach, 75% of stage 3-4 CKD patients controlled their edema within 8 weeks. Without it? Only 45% did.

What’s Next? New Tools on the Horizon
Research is moving fast. The NIH’s FOCUS trial, wrapping up in late 2025, is testing whether using bioimpedance spectroscopy (BIS) to measure fluid levels in real time can cut hospitalizations by 32%. Imagine a device that tells your doctor exactly how much fluid you’re holding-no guesswork.
Vaptans, drugs that block water retention hormones, are being studied too. But early trials showed liver damage, and one major study was halted. For now, they’re not ready for prime time.
The big shift in thinking? Slower is safer. Instead of trying to remove 2 liters of fluid in a day, doctors are now aiming for 0.5-1.0 kg (1-2 pounds) per day. That’s enough to relieve swelling without crashing kidney function.
And in 2025, the KDIGO guidelines are expected to update their recommendations-likely pushing for even tighter control of diuretic doses in advanced CKD, and more emphasis on non-drug strategies.
Can I stop taking diuretics if I cut out salt?
Some people with early-stage CKD (stages 1-3) can reduce or even stop diuretics with strict salt restriction and fluid control. But if you’re in stage 4 or 5, or have heart failure, stopping diuretics without medical supervision can be dangerous. Always talk to your nephrologist before making changes.
Why do I still swell even with diuretics?
If you’re still swollen despite diuretics, it’s likely because you’re still consuming too much salt or fluid. Diuretics can’t outwork a high-sodium diet. Also, if your kidney function has dropped too low (eGFR under 15), your body may not respond well to oral meds-injectable furosemide may be needed. Other causes include heart failure, liver disease, or protein loss from nephrotic syndrome.
Are compression socks safe for people with diabetes?
Yes, but only if you have good sensation and no open sores. Diabetics with neuropathy or poor circulation should avoid compression unless cleared by a vascular specialist. Always check your skin daily for redness, sores, or numbness. Use socks with a smooth seam and avoid ones that are too tight.
How much water should I drink if I have CKD and edema?
Most guidelines recommend limiting total fluid intake to 1,500-2,000 mL per day if you have significant edema. This includes water, tea, coffee, soup, yogurt, and even fruits with high water content. Your doctor will adjust this based on your urine output, weight, and kidney function. Don’t just rely on thirst-your body’s signal gets confused in CKD.
Can I use over-the-counter diuretics for CKD edema?
No. Over-the-counter diuretics (like herbal supplements or caffeine pills) are not safe for CKD. They can cause dangerous electrolyte shifts, worsen kidney function, and interact with prescribed meds. Only use diuretics prescribed and monitored by your nephrologist.
What to Do Next
Start with one change. Pick one of these:
- Track your sodium intake for a week using a food diary app.
- Put on your compression socks every morning before getting out of bed.
- Walk for 20 minutes after lunch-no matter how tired you feel.
Then talk to your nephrologist. Ask: “Am I on the right diuretic dose? Should I try a combination? Do I need a dietitian?” Small steps, done consistently, lead to big improvements. And in CKD, that’s everything.






13 Comments