Heart failure isn’t a single disease-it’s a cascade. It starts quietly, often without symptoms, and creeps up on you. By the time you’re breathless climbing stairs or swollen in the ankles, the damage has been building for years. But here’s the truth: heart failure is no longer a death sentence. With the right care, people aren’t just surviving-they’re living well, even with a weakened heart.
Understanding the Stages: It’s Not Just About Symptoms
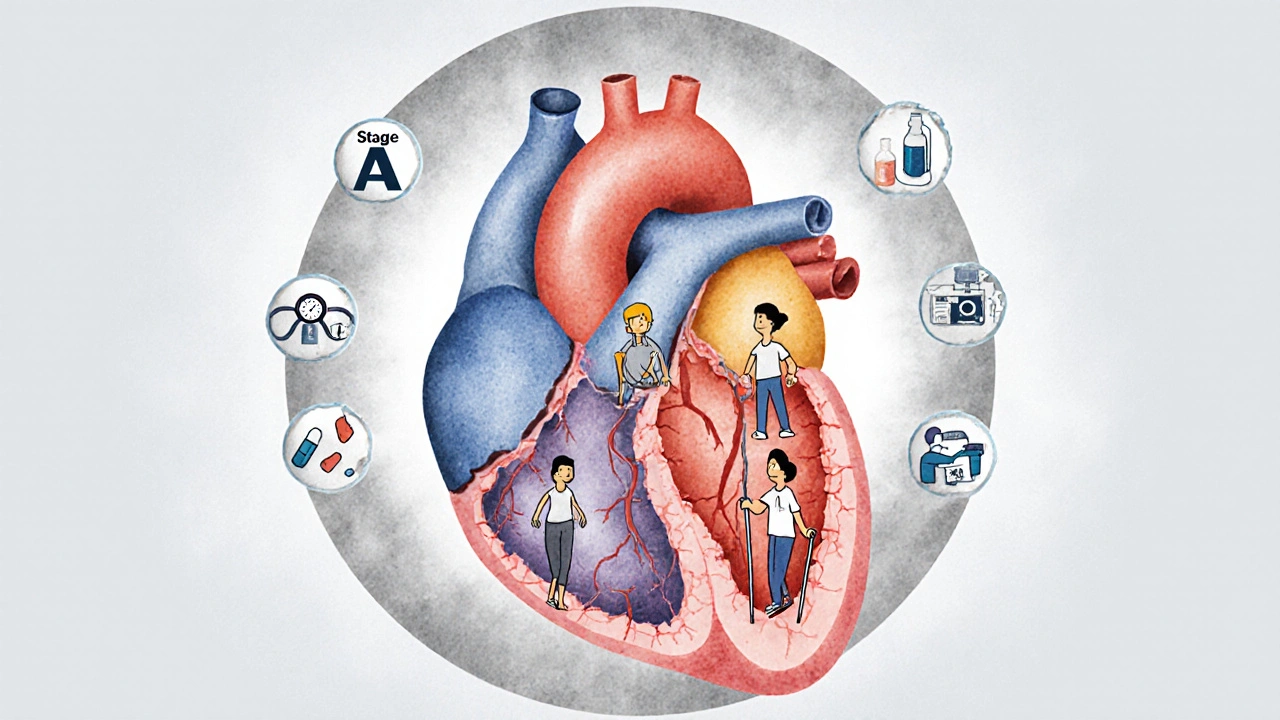
The old way of thinking about heart failure was simple: you had it, or you didn’t. Today, we know better. The 2023 American Heart Association guidelines split heart failure into four stages, from risk to advanced disease. Stage A is when you’re at risk-maybe you have high blood pressure, diabetes, or a family history-but your heart still looks normal on scans. Stage B means your heart has structural changes-maybe a past heart attack left scar tissue-but you still feel fine. Stage C is when symptoms show up: fatigue, swelling, shortness of breath. Stage D is the most serious, where standard treatments aren’t enough, and you need devices or transplants.
This staging matters because treatment changes at each step. You don’t wait until you’re gasping for air to start protecting your heart. If you’re in Stage B, taking an ACE inhibitor can cut your chance of developing full-blown heart failure by nearly half. That’s not a guess-it’s backed by data from over 300 clinical trials.
The New Gold Standard: Quadruple Therapy for HFrEF
If you’ve been diagnosed with heart failure with reduced ejection fraction (HFrEF)-meaning your heart pumps out less than 40% of its blood with each beat-you’re now on a four-drug plan. This isn’t optional. It’s the new standard. And it works.
- Sacubitril/valsartan (ARNI): Replaces older ACE inhibitors. It cuts death and hospital stays by 20% over three years.
- Carvedilol, metoprolol succinate, or bisoprolol: These beta-blockers slow your heart just enough to let it heal. They’ve been shown to cut mortality by nearly 35%.
- Spironolactone: A potassium-sparing diuretic that reduces fluid overload and protects heart muscle.
- Dapagliflozin or empagliflozin (SGLT2 inhibitors): Originally for diabetes, these drugs now help your heart beat better-even if you don’t have diabetes.
Each drug has a number attached to it: the number needed to treat (NNT). For ARNI, you need to treat 12 people to prevent one death over three years. For beta-blockers, it’s 17. That means, for every 17 people on this combo, one life is saved. That’s powerful.
And here’s the kicker: most patients don’t get all four. A 2024 study found only 39% of eligible patients received full therapy within a year. Why? Doctors worry about low blood pressure, kidney issues, or potassium spikes. But here’s the surprise: only 1.8% of heart failure patients actually have dangerously low blood pressure. Most of the time, the fear is worse than the reality.
HFpEF: The Disease That Had No Treatment-Until Now
For decades, heart failure with preserved ejection fraction (HFpEF) was a mystery. Your heart pumps fine, but it’s stiff. Fluid backs up. You’re tired. And until 2019, the only treatment was water pills. That’s it.
Then came SGLT2 inhibitors. Empagliflozin (Jardiance) and dapagliflozin (Farxiga) were tested in large trials-EMPEROR-PRESERVED and DELIVER-and they changed everything. They cut hospitalizations by nearly 20%. Patients reported more energy, less swelling, and fewer ER visits. One man in Birmingham, 74, with HFpEF told his doctor after three months on empagliflozin: “I walked to the shops yesterday. I didn’t stop once.”
These drugs aren’t magic. The absolute benefit is small-about 1.6% fewer hospitalizations over two years. But for someone who’s been hospitalized three times in a year, that’s everything.
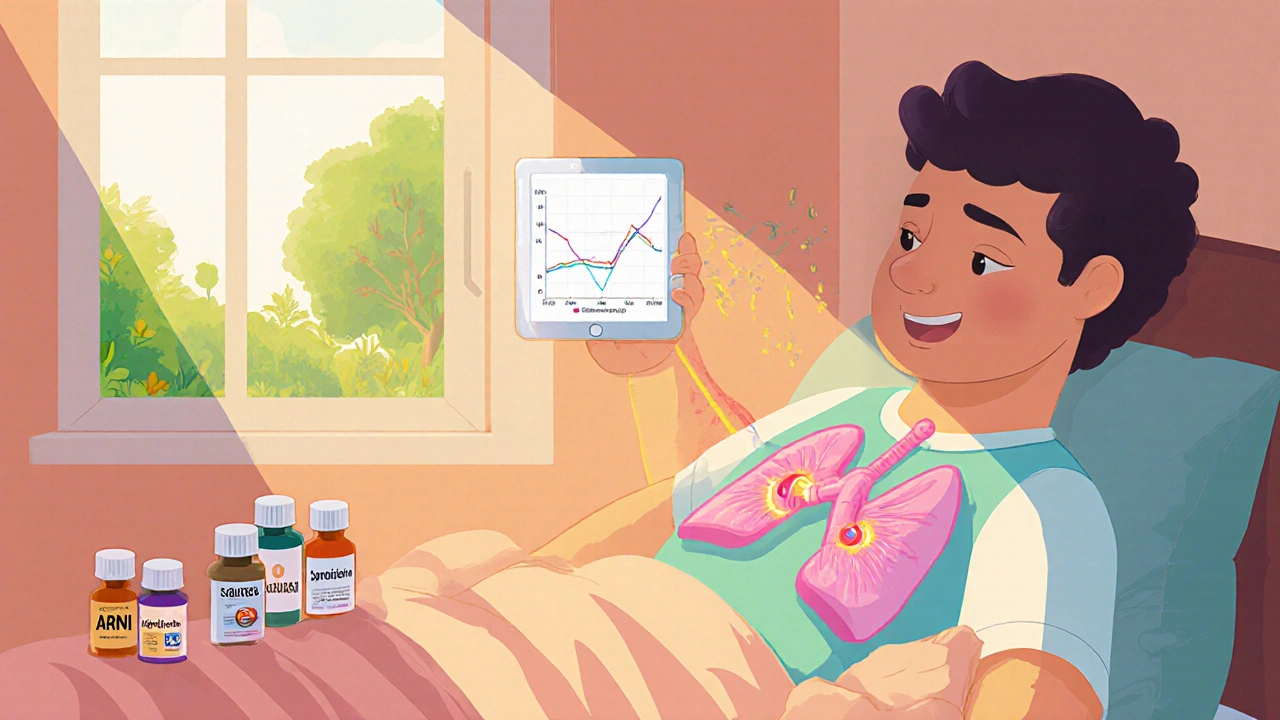
Monitoring from Inside: The CardioMEMS Device
What if you could know your heart is starting to fail before you feel it? That’s what the CardioMEMS device does. It’s a tiny sensor implanted in the pulmonary artery during a short procedure. Every day, you lie on a special pillow at home, and it wirelessly sends your lung pressure data to your care team.
Why does this matter? High pressure in the lungs means fluid is building up. If caught early, your doctor can tweak your meds before you end up in the hospital. The 2025 MONITOR-HF trial in Europe showed a 28% drop in hospital stays and better quality of life. Patients who used it said they felt more in control.
It’s not cheap-Medicare pays nearly $20,000 for the device plus quarterly monitoring. But for someone with Stage D heart failure, it can mean the difference between living at home and living in a hospital.
Why People Still Struggle: The Medication Maze
Here’s the ugly truth: managing heart failure means taking a lot of pills. The average HFrEF patient takes 7.3 medications daily. Add in drugs for diabetes, high blood pressure, or kidney disease, and it’s easy to lose track.
A 2024 survey of over 1,200 heart failure patients found 63% struggled with adherence. One caregiver wrote: “My husband has eight heart meds. I have to sort them into a pillbox every Sunday. Sometimes I still miss one.”
Doctors aren’t blameless. Many don’t know the latest guidelines. Others are afraid to push doses too high, fearing side effects. But the ACC’s “HF in a Box” toolkit-used by 42,000 providers worldwide-helps. It has checklists, patient handouts in 17 languages, and decision trees. Clinics using it saw quadruple therapy rates jump by 27% in just six months.
Disparities Still Exist
Heart failure doesn’t affect everyone equally. Black patients are 37% less likely to get guideline-recommended drugs. They’re also 28% more likely to die from it-even after adjusting for income, education, and access to care. Why? Bias, lack of trust in the system, and fewer referrals to specialists. This isn’t just a medical problem. It’s a justice problem.
Efforts are underway. Community health workers are being trained to follow up with high-risk patients. Pharmacies are offering medication reviews. But progress is slow. Real change needs systemic action-not just better drugs.
What’s Next: Personalized Care and New Frontiers
Research is moving fast. Scientists are now looking at something called CHIP-Clonal Hematopoiesis of Indeterminate Potential. It’s a genetic quirk in older adults where blood cells mutate, causing inflammation that damages the heart. About 1 in 5 people over 70 have it. And it triples heart failure risk.
A trial called INTERCEPT-HF is testing whether blocking inflammation with canakinumab can help. Another trial, TARGET-HF, is asking: should your blood pressure target depend on whether you have HFrEF or HFpEF? Early data suggests yes. One size doesn’t fit all.
And the market is booming. SGLT2 inhibitors for heart failure are now the fastest-growing drug segment. Farxiga alone captured over 40% of the HFpEF market in 2024. But the real win isn’t in sales-it’s in lives.
Living Well: It’s Possible
Heart failure management today isn’t about waiting for the next crisis. It’s about daily choices: taking your meds, weighing yourself every morning, watching your salt, walking when you can. It’s about knowing your numbers-your blood pressure, your weight, your breathing.
People aren’t just living longer. They’re living better. One woman in Birmingham, 68, with HFpEF started empagliflozin last year. She gardens again. She plays with her grandkids. She doesn’t need oxygen anymore. She didn’t get cured. But she got her life back.
That’s the new goal: not just to survive heart failure, but to thrive despite it.
Can heart failure be reversed?
In some cases, yes-especially if caught early. For people in Stage A or B, controlling high blood pressure, diabetes, or stopping alcohol can halt or even reverse heart damage. In Stage C, quadruple therapy can improve heart function significantly. Some patients see their ejection fraction climb from 25% to 50% over a year. It’s not a cure, but it’s a major recovery.
Do I need to stop all salt if I have heart failure?
You don’t need to eliminate salt completely, but you should limit it to under 2,000 mg per day. That’s about one teaspoon. Processed foods, canned soups, and restaurant meals are the biggest culprits. Read labels. Cook at home. A simple trick: use herbs, lemon, or vinegar instead of salt. Cutting salt reduces fluid buildup and lowers hospitalization risk.
Are SGLT2 inhibitors safe for people without diabetes?
Yes. Originally developed for type 2 diabetes, SGLT2 inhibitors like dapagliflozin and empagliflozin work in heart failure regardless of blood sugar levels. They help the kidneys remove extra sugar and salt, which reduces heart strain. Side effects are rare-mostly mild genital yeast infections, which are treatable. The benefits far outweigh the risks for most heart failure patients.
Why do I need so many different heart medications?
Each drug targets a different problem. ARNI reduces stress on the heart, beta-blockers slow it down, MRAs protect muscle tissue, and SGLT2 inhibitors help the kidneys and reduce inflammation. Together, they work like a team. Taking just one or two misses the full benefit. Think of it like fixing a car-you don’t just replace the tires. You check the engine, brakes, and transmission too.
What if I can’t afford my heart failure meds?
You’re not alone. Many drug manufacturers offer patient assistance programs. For example, AstraZeneca and Boehringer Ingelheim have free or low-cost options for Farxiga and Jardiance. Ask your pharmacist or care team-they can help you apply. Some clinics also have medication assistance coordinators. Never stop your meds because of cost. There are always options.
Can I exercise with heart failure?
Absolutely-when done safely. Walking, light cycling, or seated exercises improve strength, reduce fatigue, and lower hospital risk. Start slow: 10 minutes a day, three times a week. Build up gradually. Cardiac rehab programs are ideal-they’re supervised and tailored. Avoid heavy lifting or holding your breath. If you feel dizzy, chest pain, or extreme shortness of breath, stop and call your doctor.
How often should I see my doctor?
When first diagnosed or after a change in meds, you’ll need checkups every 2-4 weeks. Once stable, every 3-6 months is typical. If you use CardioMEMS, you’ll send daily readings, and your team will contact you if numbers rise. Always call sooner if you gain 2+ pounds in a day, have new swelling, or feel more breathless than usual.
Is heart failure hereditary?
Some forms are. If close family members had heart failure before age 55, especially without obvious causes like heart attacks, you may have a genetic risk. Conditions like dilated cardiomyopathy can run in families. Genetic testing is available, and if you’re at risk, your doctor may recommend earlier screening with echocardiograms.






15 Comments
Just wanted to say thanks for this. I’m a nurse in rural Ohio, and I see so many patients who don’t get the quadruple therapy because their PCP doesn’t know the guidelines. This post is the kind of thing I print and hand out. One guy on dapagliflozin went from 3 hospitalizations last year to zero. He’s gardening again. Small wins matter.
Let me guess - Big Pharma wrote this whole thing, didn’t they? SGLT2 inhibitors? They’re not ‘helping the heart’ - they’re just making kidneys dump sugar so the companies can sell more pills. And don’t get me started on CardioMEMS. That’s a surveillance tool disguised as medicine. Your lung pressure is being tracked 24/7, and who’s got access to that data? Insurance companies. Employers. The government. They’re not saving lives - they’re building a database. Wake up.
While the clinical data cited is broadly accurate, the article exhibits a troubling conflation of correlation with causation, particularly regarding the efficacy of SGLT2 inhibitors in HFpEF. The absolute risk reduction of 1.6% over two years, as acknowledged, is statistically marginal. The rhetorical framing of ‘living well’ risks infantilizing patients by implying that pharmacological intervention alone constitutes therapeutic success. A more rigorous discourse would emphasize functional capacity metrics over anecdotal testimonials - e.g., six-minute walk distance, not ‘walking to the shops.’
My dad’s on all four meds now. He used to nap after lunch. Now he plays guitar with my kids. 🎸❤️ I didn’t think he’d ever get back to that. If you’re scared of side effects? Talk to your doc. Most of the time, it’s just fear talking. He had a little dizziness at first - fixed it with a dose tweak. No big deal.
OMG I’m crying. I’ve been pushing my mom to take her meds for 3 years. She’d skip them because ‘they make me dizzy.’ Then we got her on Farxiga. She started walking to the mailbox without stopping. Now she’s dancing at my cousin’s wedding. 🥹💃 I’m so mad at every doctor who ever told her ‘it’s just aging.’ NO. IT’S NOT. This isn’t magic. It’s science. And it’s working.
So let me get this straight - you’re telling me that if I take four expensive pills, I can avoid being hospitalized? And the only reason people aren’t getting them is because doctors are ‘afraid’? That’s not fear. That’s common sense. These drugs cost $500 a month. I work two jobs and still can’t afford insulin. You think your ‘quadruple therapy’ is going to work for the guy who’s choosing between his meds and his kid’s braces? This isn’t medicine. It’s a luxury pamphlet.
It’s fascinating how the article casually dismisses the pharmacokinetic risks of combining ARNI with spironolactone without addressing the potential for hyperkalemia-induced arrhythmias. The NNT figures are cherry-picked from subgroup analyses. The MONITOR-HF trial? Underpowered. And the assertion that ‘only 1.8% have dangerously low BP’ is statistically misleading - it ignores transient hypotension, which is far more common and clinically consequential. This reads like a pharmaceutical white paper masquerading as patient education.
It is imperative to note that the author’s uncritical endorsement of SGLT2 inhibitors constitutes a profound ethical failure. These agents are associated with euglycemic diabetic ketoacidosis, genital mycotic infections, and volume depletion - all of which are non-trivial. To suggest that patients should disregard physician caution is not merely irresponsible - it is reckless. The fact that this article fails to mention the FDA’s 2023 warning regarding SGLT2 inhibitor use in patients with low BMI is unconscionable. This is not medicine. It is moral negligence.
Thank you for writing this. I’ve been living with HFpEF for 5 years. I thought I was just getting old. Turns out, I just needed the right meds. Empagliflozin didn’t fix everything - but it gave me back the mornings. I can walk to the bus stop now. That’s enough.
Let’s be real - the real ‘miracle drug’ here isn’t dapagliflozin. It’s the fact that someone finally listened to patients who said, ‘I’m not just tired - I’m drowning.’ We’ve spent decades treating symptoms, not the soul-crushing exhaustion. Now we have drugs that let people breathe again. And yes, the cost is obscene. But the silence around it? That’s worse. We need to scream louder about access - not just celebrate the science.
Oh please. ‘Living well’? That’s the new corporate euphemism for ‘you’re not dead yet.’ The article lists every fancy drug and device, but doesn’t mention that 70% of heart failure patients are over 70 and on fixed incomes. CardioMEMS costs $20K? Good luck getting Medicare to approve it when you’re 82 and live alone. This isn’t progress - it’s a marketing campaign dressed in white coats. And don’t even get me started on the ‘genetic risk’ nonsense. Next they’ll be telling us to test our blood for ‘heart failure alleles’ before we get a driver’s license.
While the clinical guidelines referenced are technically accurate, the article displays a disturbing lack of critical perspective regarding the commercial interests underpinning the dissemination of these protocols. The rapid adoption of SGLT2 inhibitors across HFpEF populations - a condition previously considered untreatable - coincides precisely with the expiration of patent protections for older diuretics. One must ask: is this paradigm shift driven by evidence, or by the profit motive of multinational pharmaceutical conglomerates? The absence of any mention of this tension is not oversight - it is complicity.
Just to clarify terminology: HFrEF and HFpEF are phenotypes, not etiologies. The quadruple therapy is effective for HFrEF, but HFpEF remains heterogeneous - subphenotypes based on obesity, hypertension, or inflammation may respond differently. SGLT2 inhibitors help, but they’re not a panacea. We need endotyping, not just staging. Also, the ‘1.6% absolute risk reduction’ sounds small, but in population-level terms? That’s tens of thousands of avoided hospitalizations. Context matters.
They say ‘heart failure isn’t a death sentence.’ Funny - my grandfather died of it in 1998. No ARNI. No CardioMEMS. Just a hospital bed and a nurse who held his hand. You call this progress? I call it overmedication wrapped in data. People don’t need more pills. They need more time - and less noise.
@4004 - you’re 100% right about the cost. I’ve been there. That’s why I used AstraZeneca’s patient program. Got Farxiga for $5 a month. My mom’s pharmacist helped us apply. It’s not perfect, but it’s something. Don’t give up. Ask. Always ask. 💪❤️