Abnormal bleeding: what’s going on and what to do first
Seeing bleeding that’s not normal for you is stressful. Whether it’s heavy periods, spotting between cycles, blood in stool or urine, or unexpected bruising, this guide helps you figure out common causes, quick first steps, and when you need urgent care.
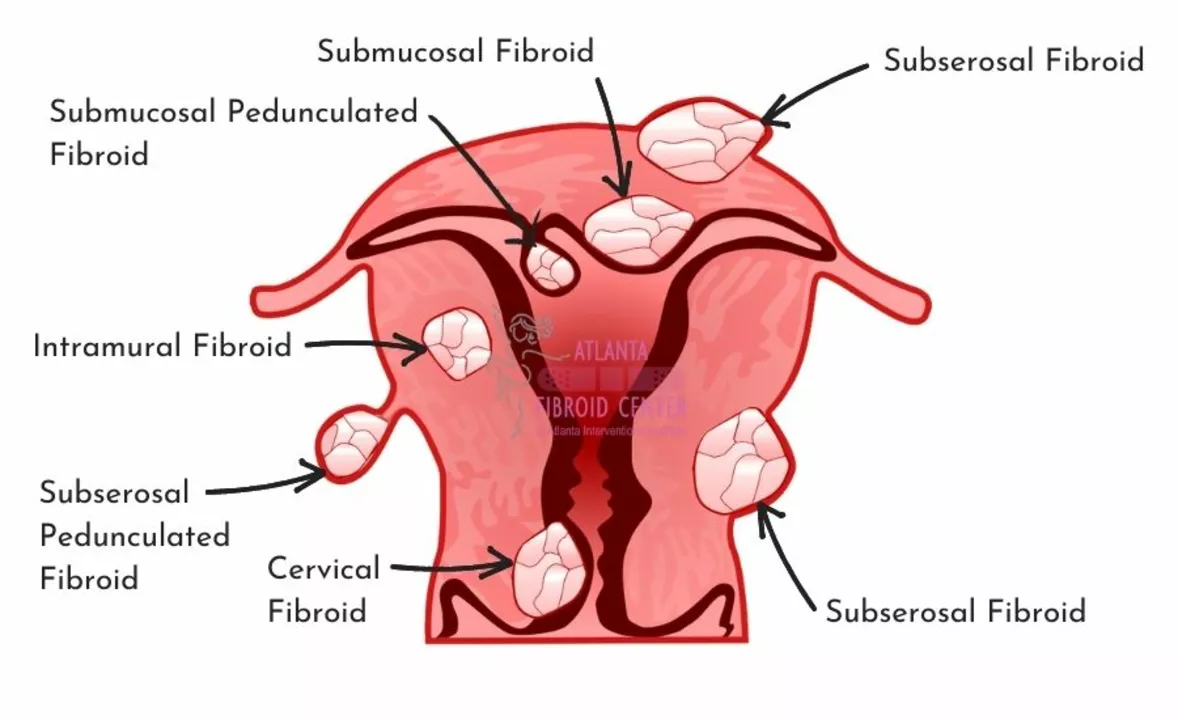
First, match the bleeding to its location. Vaginal bleeding outside your usual period can come from hormonal shifts, infections, birth control side effects, fibroids, polyps, or more serious causes like endometrial problems. Heavy, regular menstrual bleeding (menorrhagia) often points to fibroids, hormonal imbalance, or blood-clotting issues. Spotting after sex or after menopause should always be checked by a clinician.
Bleeding from the nose or mouth is usually local — dry air, trauma, or nose-picking — but repeated nosebleeds or bleeding gums can also be signs of a clotting problem or medication side effects. Blood in stool or black, tarry stools usually means bleeding in the digestive tract and needs prompt evaluation. Red blood in urine could be a urinary tract issue, kidney stones, or something more serious.
Quick, practical first steps
If bleeding is heavy, lie down and raise your legs if you feel faint. Apply direct pressure to nosebleeds. For vaginal bleeding, use pads (not tampons) and track how soaked they get—this helps medical staff judge severity. Avoid aspirin and NSAIDs if you’re bleeding, unless a provider told you to keep taking them; these drugs can make bleeding worse. Note any recent injuries, new medications (especially blood thinners), or changes in birth control.
Take photos of visible bleeding or bruises if you can’t describe them clearly later. Write down when the bleeding started, how long it lasts, and any other symptoms like dizziness, severe pain, fever, or shortness of breath. That quick timeline is often the most useful thing you can bring to an appointment.
Tests, treatment options, and red flags
Common tests include a pregnancy test, full blood count, coagulation profile, pelvic exam and ultrasound for vaginal bleeding, and stool or endoscopy studies for GI bleeding. Treatment depends on cause: hormones or tranexamic acid for heavy periods, cautery or packing for persistent nosebleeds, antibiotics for infections, and endoscopic procedures for GI bleeds. If you’re on blood thinners, your prescriber may adjust the dose or give reversal agents in emergencies.
Get emergency help if you have very heavy bleeding soaking multiple pads per hour, fainting, signs of shock (pale, cold sweat, rapid pulse), severe abdominal pain, coughing or vomiting blood, or shortness of breath. For less urgent but concerning symptoms—new heavy periods, persistent spotting, or blood in stool/urine—book a same-week appointment with your doctor.
Keeping a simple bleeding log and sharing recent medication changes will speed up diagnosis. If cost or access to local care is a worry, many clinics offer telehealth or pharmacy advice lines that can help you decide next steps. Don’t wait when bleeding is heavy or accompanied by worrying symptoms—get checked.
How Overgrowth in the Lining of the Uterus Can Lead to Abnormal Bleeding
As a blogger, I've recently been researching how overgrowth in the lining of the uterus can lead to abnormal bleeding. I discovered that this overgrowth, known as endometrial hyperplasia, can cause the uterine lining to become too thick, resulting in heavy or prolonged periods. Additionally, hormonal imbalances, such as elevated levels of estrogen without enough progesterone, can contribute to this condition. It's important to consult with a healthcare professional if you're experiencing abnormal bleeding, as it could be a sign of an underlying issue. Early detection and treatment can help prevent more severe complications, such as infertility or even cancer.
view more




