9 Jan |
20:42 PM
When your doctor suspects a kidney problem-maybe you’re in pain, have trouble urinating, or your blood tests show elevated creatinine-they often start with one simple test: renal ultrasound. It’s quick, safe, and doesn’t use radiation. But what exactly does it show? And how do doctors tell if your kidney is blocked or shrinking? This isn’t just about taking a picture. It’s about reading the signs hidden in size, shape, and blood flow.
Why Renal Ultrasound Comes First
Most hospitals and clinics start with ultrasound when checking for kidney issues. Why? Because it’s the safest option. Unlike CT scans, which expose you to radiation, or MRIs, which cost three to five times more, ultrasound uses harmless sound waves. It’s especially important for kids, pregnant women, and people who need repeated checks over time. The American College of Radiology gives it the highest rating-8 or 9 out of 9-for initial evaluation of suspected blockage. That’s higher than CT scans. Why? Because while CT can spot tiny stones, it also floods your body with radiation. A single CT urogram delivers about 10 mSv-roughly the same as 3 years of natural background radiation. Ultrasound gives you the same critical info without the risk. Emergency departments use it daily. In fact, point-of-care ultrasound at the bedside cuts diagnosis time for kidney stones by nearly 45 minutes. That’s huge when someone’s in agony. And for patients with known obstructions, like after UPJ surgery, doctors track changes week after week with ultrasound instead of ordering repeat CTs.What the Machine Measures: Size, Shape, and Flow
A renal ultrasound doesn’t just show if your kidney looks big or small. It gives you precise numbers. For adults, a normal kidney is 9 to 13 centimeters long. Anything shorter than 9 cm might mean chronic damage. Cortical thickness-the outer layer of the kidney-should be over 1 cm. If it’s thinner, your kidney may have been under stress for a long time. The renal pelvis, where urine collects before moving to the ureter, should measure less than 7 mm. If it’s wider, that’s hydronephrosis-urine backing up because something’s blocking its path. Doctors grade this from mild to severe using the Society for Fetal Urology scale. Mild means a slight bulge. Severe means the whole kidney is swollen like a water balloon. But size alone doesn’t tell the full story. That’s where Doppler ultrasound comes in. It measures blood flow through the kidney’s arteries. The key number here is the resistive index (RI). It’s calculated from the speed of blood flow during heartbeats. A normal RI is below 0.70. If it’s 0.70 or higher, there’s a strong chance of obstruction. One 2015 study showed this method was 86.7% sensitive and 90% specific for detecting blockages. That’s why experienced radiologists don’t just look at pictures-they look at waveforms. They take at least three clean measurements from the interlobar arteries, using a 1mm sample gate. It’s not guesswork. It’s math.How Ultrasound Finds Obstruction
Obstruction can happen anywhere: at the kidney’s outlet (UPJ), in the ureter, or near the bladder. Ultrasound spots the effects, not always the cause. For example, if one kidney is swollen and the other isn’t, the problem is likely on the swollen side. If both are swollen, it could be a blockage lower down, like a stone in the ureter or an enlarged prostate. Ultrasound can also detect things CT misses. For instance, it can show a blood vessel crossing over the ureter-something that squeezes it shut in UPJ obstruction. That’s called a crossing vessel, and it’s a common cause of obstruction in children. CT scans don’t show this well. Ultrasound does. Newer techniques like shear-wave elastography are starting to show up in research labs. These measure how stiff the kidney tissue is. When urine backs up, pressure builds. That pressure makes the kidney harder. In preclinical models, researchers saw a direct link: more pressure = more stiffness. This could one day let doctors grade obstruction by feel-not just by size.
Where Ultrasound Falls Short
Ultrasound isn’t perfect. It can’t see small stones. If a stone is under 3 mm, it often disappears on ultrasound. CT catches those. So if you have severe pain and ultrasound shows nothing, your doctor might still order a CT. Obesity is another big problem. If your BMI is above 35, sound waves struggle to reach the kidneys. The image gets blurry. In those cases, doctors have to switch to MRI or CT-even though they’d rather avoid it. Ultrasound also doesn’t tell you how fast urine is draining. That’s something CT with special software can measure. But that’s expensive and involves radiation. So for most patients, doctors rely on serial ultrasounds over days or weeks to see if the swelling is getting worse or better. And then there’s the human factor. Studies show up to 20% variation in kidney measurements between inexperienced and expert sonographers. That’s why training matters. The American Institute of Ultrasound in Medicine requires 40 supervised exams before certification. Many radiology residents say it takes about 50 exams to feel confident measuring resistive index correctly.What Happens After the Scan
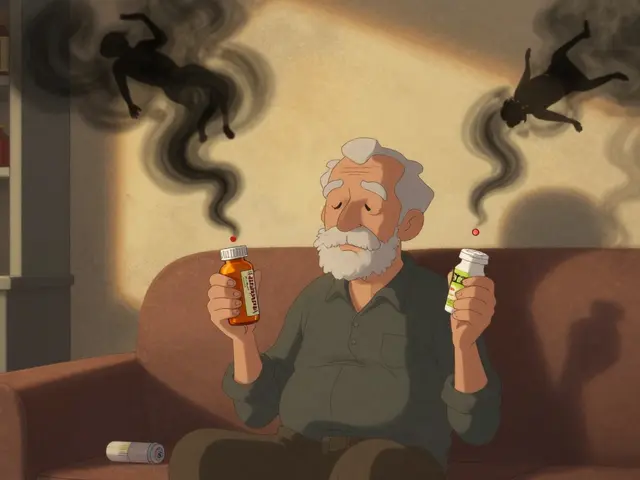
If your ultrasound shows mild hydronephrosis and no other issues, your doctor might just watch and wait. They’ll schedule a repeat scan in 4 to 6 weeks. If it’s stable, no action is needed. If it’s getting worse, they’ll look for the cause: a stone, a tumor, or a narrowing. If the resistive index is high and the kidney is swollen, they’ll move faster. They might order a diuretic renogram-a nuclear test that shows how well the kidney drains. Or they might use MRI urography for a detailed look at the ureters. In some cases, they’ll use ultrasound to guide a procedure. For example, if a kidney is severely blocked and infected, they might insert a tiny tube (nephrostomy) directly into the kidney to drain it. Ultrasound helps them do that safely without cutting.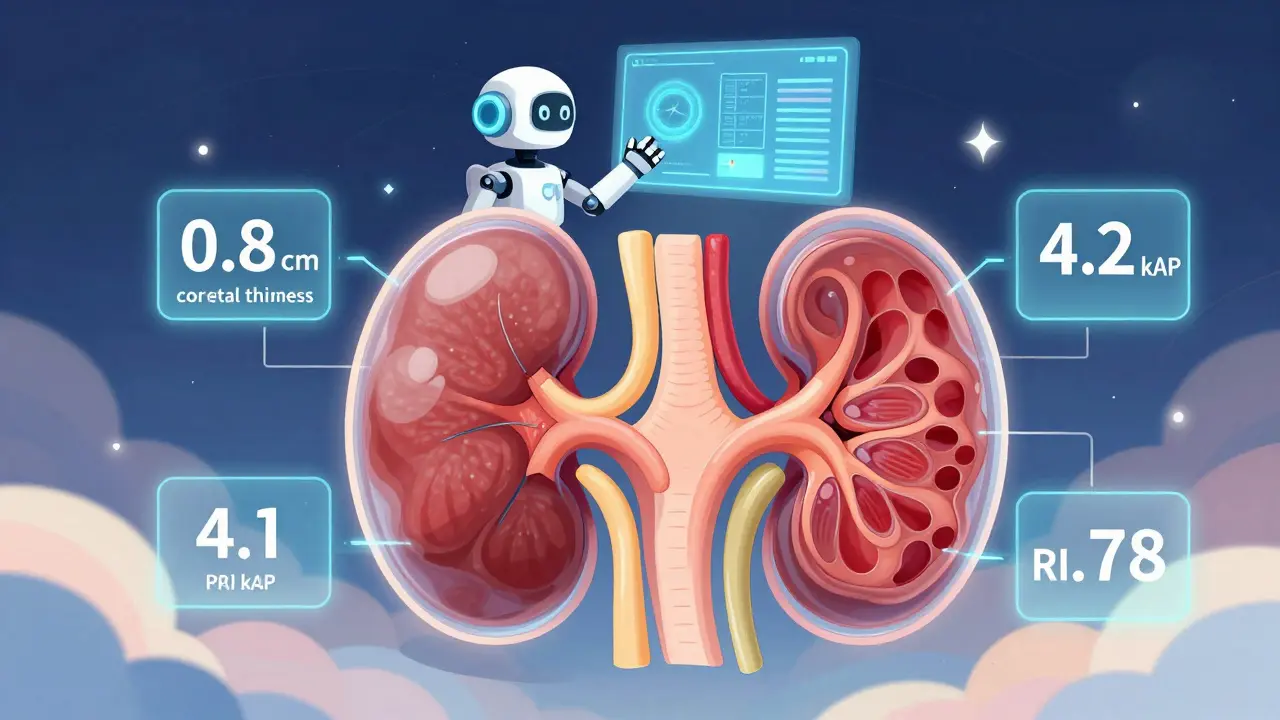



13 Comments
Love how this breaks down renal ultrasound like a streetwise doctor explaining it over chai. In India, we don’t always have CT machines handy, so this stuff? Lifesaver. Saw a cousin get diagnosed with a tiny stone just from a portable ultrasound at a rural clinic-no radiation, no panic, just calm answers. Thanks for the clarity.
so like… ultrasound is the ‘i’m too broke for a ct’ diagnostic? cool. guess we’re just gonna stare at blurry blobs and hope the radiologist didn’t nap through med school. also, 10 msv of radiation? that’s just a cosmic coffee break. i’d rather be a radioactive zombie than risk misdiagnosis by someone who thinks ‘resistive index’ is a new brand of energy drink.
How quaint. We used to rely on the divine intuition of sonographers in the 80s. Now we have algorithms and resistive indices-how dreadfully scientific. One wonders if the next evolution will be ultrasound guided by astrology or perhaps a horoscope-based cortical thickness estimator. Truly, progress.
Hydronephrosis grading via SFU scale? RI thresholds at 0.70? This is standard-of-care, but nobody talks about inter-operator variability. If you're not using a standardized protocol with intercostal vs. subcostal approaches, your data is noise. And don’t even get me started on BMI >35-obesity isn’t a comorbidity, it’s a diagnostic dead end.
So… you’re telling me we’re using math on sound waves to avoid radiation… but we still can’t see 3mm stones? That’s like using a magnifying glass to find a grain of sand in a sandcastle. I get the safety angle, but isn’t this just delaying the inevitable? If you’re in pain and ultrasound says ‘maybe,’ doesn’t that just mean you’re stuck waiting for the CT to hurt worse?
Really appreciate this breakdown! 🙌 I’m a med student in Delhi and we barely touch Doppler in our rotations. This made me go back and rewatch my ultrasound lab videos. The part about crossing vessels in kids? Mind blown. Also, 40 supervised exams to get certified? That’s more than I’ve done on my phone this week 😅
Ultrasound is a glorified guess. You think a 0.70 RI means obstruction? Try telling that to a patient with a 3mm stone that vanished on the scan. Radiologists are overpaid guessers with a fancy machine. And ‘quantitative biomarkers’? That’s just corporate jargon for ‘we still don’t know what we’re looking at.’
Wait-so you’re telling me that ultrasound is ‘safe’… but if I’m obese, I get radiation? And if I’m poor, I get blurry images? And if I’m lucky, some overworked tech with 12 exams under their belt will ‘eyeball’ my kidney?!!! This isn’t medicine-it’s a lottery with kidneys as the prize. I’m not a patient. I’m a statistical outlier waiting to be misclassified.
Ultrasound is fine if you’re not sick
This is beautiful. In Nigeria, we use ultrasound because it’s all we have-and it works. I saw a man with a blocked kidney get a tube placed with ultrasound guidance. No hospital, no fancy machine, just a skilled tech and a quiet room. This post reminds me that good care doesn’t need expensive tools. Just good hands and good eyes.
Okay so I read this whole thing and I think… maybe ultrasound is good? But I’m not sure because I think the resistive index thing is confusing and also I think the part about shear wave elastography is cool but I don’t know what kPa means and also why is the cortex thinner if it’s damaged? Like… is it just shrinking? Or is it dying? I’m just a patient. I don’t need all this. Can someone just tell me if I need a CT or not??
OMG I just had a renal ultrasound last week and I was terrified! But reading this made me feel so much better. I didn’t realize they were measuring the blood flow too-I thought it was just pictures. And the part about ‘water balloon kidney’? That’s literally how I described it to my mom. Thank you for making this feel human 💖
Quantitative ultrasound biomarkers represent a paradigm shift in non-invasive renal assessment. The integration of resistive index, cortical thickness, and parenchymal stiffness into a unified diagnostic metric aligns with emerging standards in precision nephrology. However, the clinical applicability remains constrained by inter-scan variability and lack of longitudinal validation cohorts. Further prospective studies are required to establish inter-institutional reproducibility before widespread adoption.