SSRI-NSAID Risk Assessment Calculator
Risk Assessment Tool
This tool estimates your risk of gastrointestinal bleeding when taking both an SSRI (antidepressant) and an NSAID (pain reliever) together. Based on your inputs, it will calculate your risk level and provide recommendations.
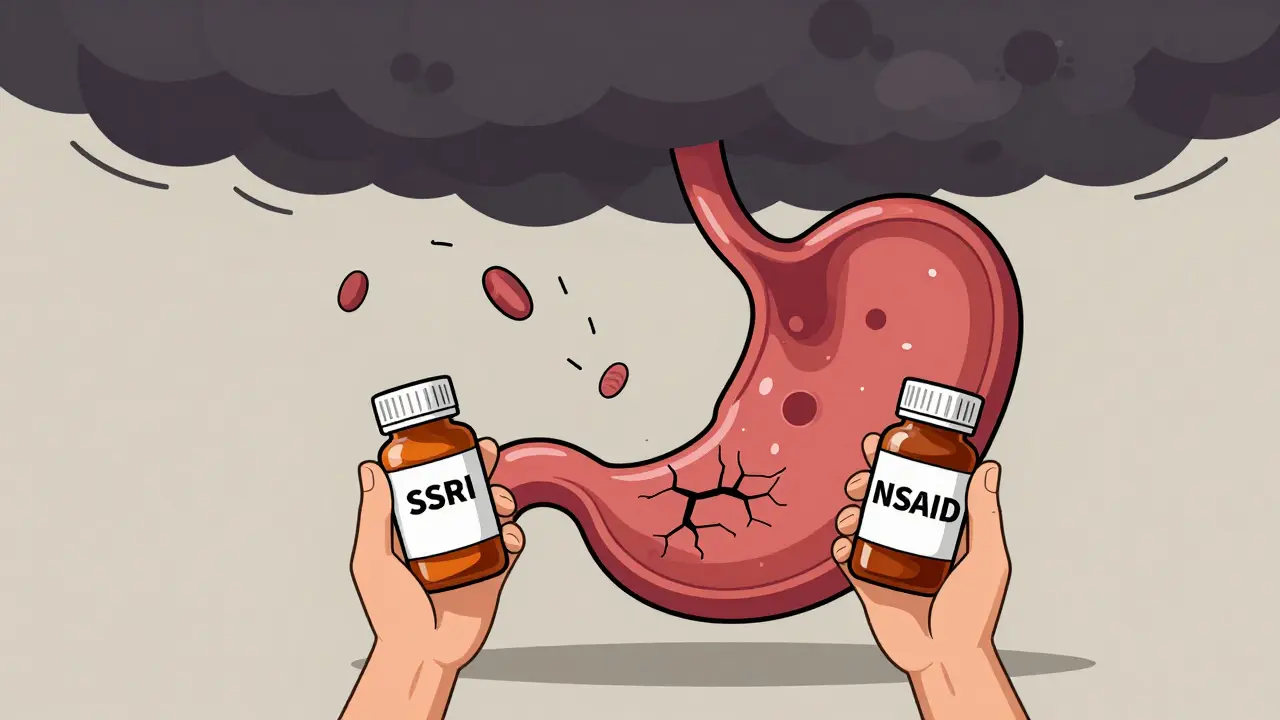
When you're managing chronic pain and depression at the same time, it’s easy to assume your doctor has checked all the boxes. But one dangerous combination slips through the cracks far too often: SSRIs and NSAIDs. Together, they don’t just add up - they multiply risk. And most people, even those who see doctors regularly, have no idea.
Think about it: nearly 1 in 8 adults in the U.S. takes an SSRI like sertraline, fluoxetine, or escitalopram. Nearly 1 in 6 takes an NSAID like ibuprofen, naproxen, or diclofenac for back pain, arthritis, or headaches. When you combine them, your chance of a serious gastrointestinal bleed jumps by 75% compared to taking NSAIDs alone. That’s not a small bump. That’s the difference between a 1% risk and a 1.75% risk - and when you’re talking about millions of people, that’s tens of thousands of emergency room visits every year.
Why This Combo Is So Dangerous
It’s not just one thing going wrong. It’s two separate systems failing at once.
SSRIs work by increasing serotonin in the brain to improve mood. But serotonin isn’t just a brain chemical. Platelets - the cells that help your blood clot - rely on serotonin to stick together and stop bleeding. SSRIs block the serotonin transporter in platelets, leaving them sluggish. They can’t aggregate properly. So if you get a tiny tear in your stomach lining, your body can’t seal it fast enough.
Meanwhile, NSAIDs attack the stomach’s natural defenses. They block enzymes (COX-1) that make protective prostaglandins. Without those, your stomach lining becomes thin, raw, and vulnerable. Even a little acid can start a small ulcer. Combine that with platelets that won’t clot, and you’ve got a perfect storm.
This isn’t theoretical. A 2022 meta-analysis of over 1.2 million patients confirmed the 75% increased risk. The data doesn’t lie. And it gets worse with age. If you’re over 65, have a history of ulcers, or take blood thinners like aspirin on top of this combo? Your risk shoots up more than 12 times compared to someone taking neither.
Not All SSRIs or NSAIDs Are Equal
Some drugs in these classes are riskier than others.
Among SSRIs, paroxetine and fluoxetine have the strongest effect on platelet serotonin uptake. That means they’re more likely to interfere with clotting. Sertraline and citalopram are a bit gentler on platelets - but still not safe when paired with NSAIDs.
For NSAIDs, the story is clearer. Non-selective ones like naproxen and diclofenac are the worst offenders. Ibuprofen is a bit better, but still risky. Celecoxib, a COX-2 selective NSAID, has significantly lower bleeding risk - about half that of naproxen. But it’s not risk-free. And it’s more expensive. So switching isn’t always simple.
Here’s the real kicker: acetaminophen (paracetamol) doesn’t touch your stomach lining or platelets. It doesn’t interact with SSRIs. For pain relief, it’s the safest bet if you’re on an antidepressant. Many patients don’t know this. They assume all painkillers are the same. They’re not.
What Doctors Should Do - But Often Don’t
Guidelines from the American Gastroenterological Association are clear: if you’re on both an SSRI and an NSAID, you need a proton pump inhibitor (PPI) like omeprazole or pantoprazole. PPIs reduce stomach acid and help the lining heal. Studies show they cut bleeding risk by about 70%.
But here’s the problem: most doctors don’t think about it. A 2021 study found that in 28% of cases, primary care doctors prescribed SSRIs and NSAIDs together without any protective medication. Even after education programs, 9% still did. That’s nearly 1 in 10 patients being left exposed.
Why? Because the risk feels abstract. Patients don’t come in bleeding. They come in with a headache and low mood. The doctor prescribes ibuprofen and sertraline. No red flags. No warning. No follow-up. And six months later, they show up in the ER with black stools and low blood pressure. By then, it’s too late.
One patient on Reddit wrote: “I was on sertraline and ibuprofen for six months. No one told me this could cause bleeding. I ended up in the hospital with a GI bleed. I lost 3 units of blood.” That’s not rare. It’s predictable.

Who’s at Highest Risk?
Not everyone needs a PPI. But some people absolutely do. Here’s who:
- Age 65 or older
- History of stomach ulcers or GI bleeding
- Taking low-dose aspirin (even 81 mg daily)
- On corticosteroids or anticoagulants
- Has kidney disease or liver problems
- Uses NSAIDs regularly (more than 10 days a month)
- Has been on an SSRI for more than 90 days
If you check even one of these boxes, you’re in the danger zone. The AIMS65 score - a simple tool doctors can use - helps predict who’s most likely to bleed. It looks at albumin levels, INR, mental status, blood pressure, and age. If you score 2 or higher, you need a PPI. No exceptions.
What You Can Do Right Now
You don’t have to wait for your doctor to bring it up. Here’s what to do:
- Ask if you really need the NSAID. Can you switch to acetaminophen? For most types of pain - headaches, muscle aches, joint stiffness - acetaminophen works just as well without the bleeding risk.
- If you must keep the NSAID, ask for a PPI. Don’t accept “it’s probably fine.” Say: “I’m on an SSRI. I’ve read this combination can cause bleeding. Can you prescribe me omeprazole 20 mg daily?”
- Know the warning signs. Black, tarry stools. Vomiting blood or material that looks like coffee grounds. Sudden dizziness, weakness, or rapid heartbeat. These aren’t normal. Call your doctor or go to the ER.
- Check your meds. Look at your pill bottles. If you’re taking more than one NSAID (like Advil and Aleve), stop one. If you’re taking aspirin for heart health and also an SSRI, talk to your doctor about whether you still need it.
- Bring your full list to every appointment. Don’t assume your doctor knows everything you’re taking. Many patients don’t mention OTC drugs. But ibuprofen from the pharmacy counts just as much as a prescription.

What’s Changing in 2026
The system is slowly waking up. Since 2019, the FDA has required all SSRI labels to include warnings about NSAID interactions. In 2023, Epic EHR systems started rolling out a GI-BLEED risk calculator that flags patients on this combo and recommends PPIs automatically. Hospitals in the U.S. and U.K. are seeing a 32% drop in bleeding events since implementing these alerts.
Pharmacies are starting to catch on too. Some now flag SSRI-NSAID combinations at the point of sale and offer a free 7-day PPI sample. Insurance companies are pushing back on prescribing naproxen to SSRI users without a PPI - and approving acetaminophen as a first-line option.
And new antidepressants are coming. Vortioxetine, approved in 2021, shows 40% less platelet interference than traditional SSRIs. Lumateperone, a newer option, may offer antidepressant effects without touching serotonin in platelets at all. These aren’t widely used yet - but they’re the future.
The Bottom Line
This isn’t about fear. It’s about awareness. You can treat depression and pain. You just can’t do it with the same old combo without protection.
SSRIs save lives. NSAIDs relieve suffering. But together, without a plan, they can put you in the hospital. The solution isn’t complicated: ditch the NSAID if you can. If you can’t, take a PPI. And always - always - ask your doctor about bleeding risk before adding any new pill to your routine.
It’s not a big ask. Just one question: “Could this interact with my antidepressant?” That’s all it takes to avoid a life-altering event.






10 Comments
Thank you for writing this. I’ve been on sertraline for 3 years and ibuprofen for my back pain for just as long - no one ever mentioned this risk. I just switched to acetaminophen last week after reading this, and honestly? My pain is still manageable. I feel like I just dodged a bullet. Please share this with your doctor, your mom, your yoga buddy - anyone who takes pills for anything. We need more awareness like this.
So let me get this straight - we’re telling people to stop NSAIDs because of a 0.75% absolute risk increase? Meanwhile, we’re prescribing opioids for chronic pain like they’re candy. The system is broken. PPIs are cheap, easy, and effective - why isn’t this automated in every EHR? Because profit > patient safety. Again.
Wow. Another fearmongering article that ignores the fact that 99.25% of people on this combo don’t bleed. If you’re gonna scare people, at least cite the NNT. 1 in 133 people on this combo get a bleed over a year? That’s less than getting hit by lightning. Stop weaponizing medical anxiety. Also, acetaminophen kills your liver if you take it wrong - guess what? You didn’t mention that. Hypocrite.
This is a critical piece of information that is systematically neglected in clinical practice, particularly in resource-constrained settings. In India, where over-the-counter NSAIDs are consumed without prescription and SSRIs are increasingly prescribed by general practitioners, the confluence of these two drug classes represents a silent public health crisis. The absence of pharmacist counseling and digital decision-support tools exacerbates the risk. A structured intervention - perhaps even a mandatory alert at the point of sale - is not merely advisable, it is ethically imperative.
Wait… so… SSRIs… affect platelets? And NSAIDs… damage the stomach lining? And together… it’s worse? I mean… I knew they were both bad… but not like… this bad? I’m on sertraline and naproxen… I think I’m gonna go see my doctor tomorrow… I didn’t even know… this was a thing…
Isn’t it ironic? We medicate the mind to escape pain, then medicate the body to ignore it - and in doing so, we destroy the very vessel that holds both. The body is not a machine to be patched. It is a temple of signals, and we are deaf to its whispers until it screams. Perhaps the real illness is our refusal to sit with discomfort - and instead, reach for another pill.
my doc gave me zoloft and advil for my anxiety and bad knees. never said a word. i just started taking tylenol and honestly? i feel way better. not just physically - like, mentally too? maybe because i’m not scared i’m gonna bleed out? weird. but good.
AMERICA IS DROWNING IN PILL POPPING AND DOCTORS WHO DON’T CARE. THIS IS WHY WE CAN’T HAVE NICE THINGS. EVERYTHING IS A COMMODITY. EVEN YOUR STOMACH LINING. THEY’RE SELLING YOU DEATH AND CALLING IT HEALTHCARE. I’M SO SICK OF THIS. 🇺🇸💔
The 75% relative risk increase is statistically significant, but clinically, the absolute risk remains low in low-risk cohorts. However, in patients with comorbidities - particularly those with elevated INR, hypoalbuminemia, or renal impairment - the pharmacodynamic synergy between SSRIs and non-selective NSAIDs creates a high-risk phenotype. PPI prophylaxis is indicated in this population per ACG guidelines, and failure to implement it constitutes a breach of the standard of care. The absence of EHR integration remains a systemic failure.
Why do doctors even exist if they don’t tell you stuff like this? I’m just mad. I could’ve died. And no one said anything. I’m not even mad at my doctor - I’m mad at the whole system. It’s broken.