Thyroid Risk Calculator for Lithium Users
Assess Your Thyroid Risk on Lithium
This tool helps you understand your personal risk of developing thyroid issues while taking lithium for bipolar disorder. Your results will help you discuss monitoring needs with your doctor.
Your Thyroid Risk Assessment
Recommended monitoring schedule:
When you're managing bipolar disorder, lithium can be a lifeline. It’s one of the oldest and most effective mood stabilizers we have, proven to cut suicide risk and prevent both manic and depressive episodes. But for many people, that benefit comes with an unexpected cost: your thyroid starts to struggle. It’s not rare. About one in five people on long-term lithium develop hypothyroidism. Some get goiters. A few even experience sudden hyperthyroidism. And if you don’t know what’s happening, you might blame fatigue, weight gain, or brain fog on your mental health - when it’s actually your thyroid.
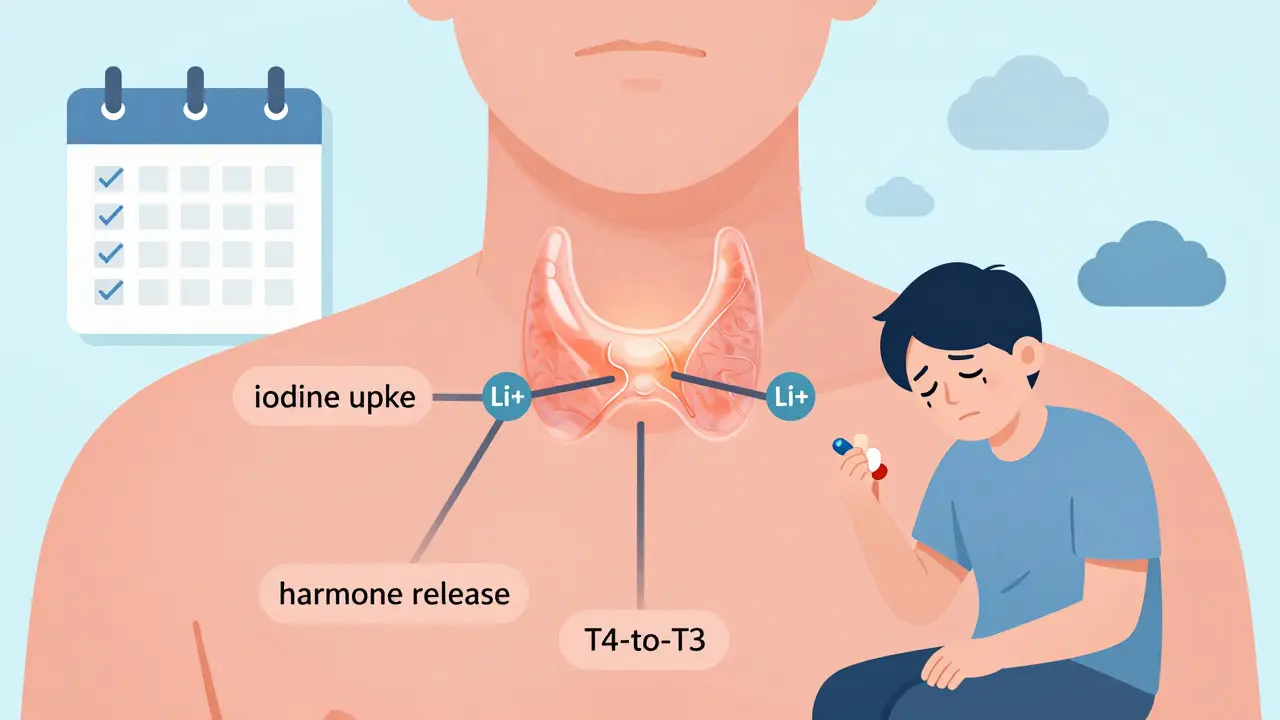
How Lithium Messes With Your Thyroid
Lithium doesn’t just float through your body. It actively interferes with how your thyroid works. The thyroid makes hormones that control your metabolism, energy, and mood. Lithium blocks three key steps in that process: it stops iodine from being used to make thyroid hormones, it prevents the gland from releasing the hormones it’s already made, and it slows down how your body converts the main hormone (T4) into the active form (T3). Over time, this leads to lower hormone levels - and that’s hypothyroidism.It also causes your thyroid to swell. About 40% of people on lithium develop a goiter - a visible or palpable enlargement of the gland. This isn’t cancer. It’s not always even uncomfortable. But it’s a sign your thyroid is working overtime just to keep up. The risk goes up with how long you’ve been on lithium. After 10 years, nearly half of users show thyroid changes. Women under 60 are at especially high risk - they’re more than three times as likely as men to develop problems on the same dose.
Hypothyroidism: The Most Common Problem
If your TSH (thyroid-stimulating hormone) climbs above 4.5 or 5.0 mIU/L, that’s a red flag. Many patients don’t notice symptoms at first. Fatigue, dry skin, constipation, cold hands, and unexplained weight gain are easy to brush off as stress or aging. But when you’re on lithium, these aren’t just lifestyle issues - they’re biological signals.Studies show that about 32% of people on long-term lithium end up needing thyroid hormone replacement. That’s usually levothyroxine, a simple daily pill. But here’s the catch: people on lithium often need higher doses than others with the same TSH levels. Why? Because lithium interferes with how well the body absorbs and uses the medication. One study found patients needed 20-30% more levothyroxine just to get their TSH into the normal range.
And here’s something many doctors miss: it takes 6 to 8 weeks after starting lithium before your TSH even begins to rise. So if your doctor checks your thyroid at week 4 and says you’re fine, they’re too early. Waiting until the 3-month mark gives a clearer picture. Still, too many primary care providers panic at a slightly high TSH and stop lithium altogether - even though the problem is fixable with medication. A 2022 study found 23% of patients had their lithium discontinued unnecessarily because of this misunderstanding.
Hyperthyroidism: Less Common, But Dangerous
About 3-5% of lithium users develop hyperthyroidism. It’s not usually Graves’ disease (an autoimmune condition). More often, it’s painless thyroiditis - where the thyroid gets inflamed and leaks stored hormones into the bloodstream. This causes temporary symptoms like rapid heartbeat, anxiety, weight loss, and sweating. It’s scary, but it usually resolves on its own in 3 to 6 months. No antithyroid drugs are needed.But there’s a dangerous twist. If you’ve been on lithium for years and suddenly stop - whether because of toxicity, surgery, or a decision to switch meds - your thyroid can go into overdrive. There’s only one documented case of thyroid storm (a life-threatening surge of hormones) after lithium was removed via dialysis. But it’s enough to warn doctors: never stop lithium abruptly if you’ve been on it for more than a year. Taper slowly, and monitor thyroid levels closely.

How Lithium Compares to Other Mood Stabilizers
Not all mood stabilizers hit the thyroid the same way. Valproate can cause mild TSH spikes in 5-10% of users, but it rarely leads to full-blown hypothyroidism. Carbamazepine? Almost no effect. Lithium stands out because it doesn’t just nudge the thyroid - it rewires how it functions. That’s why, despite newer drugs being available, lithium remains first-line treatment for bipolar I disorder. It’s still the most effective at preventing suicide and long-term mood episodes.A 2017 meta-analysis showed lithium reduces the risk of any mood episode by 39% compared to placebo. No other drug matches that. Even with thyroid problems, many patients say: “I’d rather take levothyroxine than go back to cycling between mania and depression.” On Reddit, 41% of positive reviews said exactly that. The trade-off is worth it - if you’re monitored properly.
Who’s at Highest Risk?
Not everyone on lithium gets thyroid issues. But some groups are far more vulnerable:- Women under 60 - 3.2 times more likely than men
- People with a family history of thyroid disease
- Those with existing autoimmune conditions (like Hashimoto’s)
- Patients on higher doses (over 900 mg/day)
- People living in low-iodine regions - goiter rates are higher in Denmark than in the U.S.
And dose matters. A 2024 study found that for every 100 mg increase in daily lithium dose, your odds of thyroid dysfunction go up by 27%. That doesn’t mean you can’t take a higher dose if needed - but it does mean you need tighter monitoring.
What You Should Do: A Clear Monitoring Plan
The American Thyroid Association says it plainly: test before you start, then every 6 months for the first year, then annually. That’s non-negotiable.Here’s what your bloodwork should include:
- TSH (thyroid-stimulating hormone)
- Free T4
- Free T3 (if TSH is abnormal)
- Thyroid antibodies (TPOAb) - only if you have symptoms or family history
Don’t rely on TSH alone. Some patients have normal TSH but low free T4 - that’s still hypothyroidism. And if you’re on levothyroxine, check levels 6-8 weeks after any dose change. Lithium can make your body respond slower to adjustments.
New Hope: Selenium and Future Treatments
There’s good news on the horizon. A 2023 clinical trial gave 100 mcg of selenium daily to lithium users. After two years, the rate of hypothyroidism dropped from 24% to 14%. Selenium helps protect the thyroid from oxidative stress - a side effect of lithium’s interference. It’s not a cure, but it’s a simple, safe addition that could prevent a lot of suffering.Researchers are also working on lithium alternatives that don’t hurt the thyroid. RG101, currently in Phase II trials, looks promising. It stabilizes mood just as well as lithium but doesn’t raise TSH. If it works, it could change everything.
What to Do If You’re Already on Lithium
If you’re taking lithium and feel off - tired, heavy, cold, gaining weight - don’t assume it’s your bipolar disorder. Get your thyroid checked. Ask for TSH and free T4. If your doctor says “it’s probably just stress,” push back. Bring up the data: 32% of people on lithium develop thyroid issues. That’s not normal - it’s expected.If you’re diagnosed with hypothyroidism, take your levothyroxine exactly as prescribed. Don’t skip doses. Don’t switch brands without checking your levels. And don’t be afraid to ask your psychiatrist: “Can we lower my lithium dose if my thyroid is stable?” Some patients do well on lower doses once their thyroid is managed.
And if you’re thinking about stopping lithium? Talk to your doctor first. Don’t quit cold turkey. The risk of rebound hyperthyroidism or even thyroid storm is real. Work with your team to make a safe plan.
Living Well With Lithium and Thyroid Issues
You don’t have to choose between mental stability and physical health. Most people on lithium who develop thyroid problems can live full, active lives - as long as they’re monitored. I’ve seen patients who’ve been on lithium for 15 years, on levothyroxine, with perfect mood control and normal thyroid levels. It’s not perfect. But it’s manageable.Keep your appointments. Track your symptoms. Eat a balanced diet with enough iodine (seafood, dairy, eggs). Avoid excessive soy or cruciferous vegetables if you’re hypothyroid - they can interfere with absorption. And if you ever feel your mood slipping, don’t blame your thyroid. Check both. Because when lithium and your thyroid are working together, you’re not just surviving - you’re living.
Does lithium always cause thyroid problems?
No. About 20-32% of people on long-term lithium develop thyroid dysfunction, mostly hypothyroidism. Many others never have issues. Risk depends on dose, gender, age, iodine intake, and genetics. Regular blood tests catch problems early, so you can treat them before they affect your daily life.
Can I stop lithium if my thyroid gets bad?
Don’t stop lithium on your own. Stopping suddenly can trigger hyperthyroidism or even thyroid storm - a life-threatening condition. If your thyroid problems are severe, work with your psychiatrist and endocrinologist to lower your lithium dose slowly while starting or adjusting thyroid medication. In many cases, you can stay on lithium safely with proper management.
Will levothyroxine fix all my symptoms?
Most symptoms improve - fatigue, weight gain, cold intolerance. But some people still feel off even with normal TSH levels. That’s because lithium affects more than just thyroid hormone levels - it can alter how your brain responds to hormones. If you’re still tired after 3-6 months on levothyroxine, ask about free T3 testing or selenium supplementation. You’re not imagining it.
How often should I get my thyroid checked on lithium?
Baseline test before starting, then every 6 months for the first year. After that, once a year if your levels are stable. If you’re on levothyroxine, check every 6-8 weeks after a dose change. Women, older adults, and those on higher doses may need more frequent checks. Don’t wait for symptoms - get tested.
Can selenium help prevent thyroid issues on lithium?
Yes. A 2023 study showed 100 mcg of selenium daily reduced hypothyroidism risk from 24% to 14% over two years in lithium users. It’s safe, inexpensive, and available over the counter. Talk to your doctor about adding it - especially if you’re at high risk or already have mild thyroid changes.
Is lithium still worth taking if it affects my thyroid?
For many people, yes. Lithium reduces suicide risk by 14% more than other mood stabilizers. It’s the most effective at preventing long-term mood episodes. If you can manage thyroid side effects with routine monitoring and levothyroxine, the benefits usually outweigh the risks. Most patients who stick with it say they wouldn’t trade their mood stability for the thyroid issues.






8 Comments
lithium saved my life but my thyroid went full zombie mode after 3 years
doc said just take levothyroxine and i did
now i feel like a human again not some zombie dragging through work
also selenium? i started taking it and my skin stopped looking like cracked desert sand
so let me get this straight - you’re telling me the only drug that actually stops people from killing themselves comes with a side effect that turns your thyroid into a confused alarm clock?
brilliant. just brilliant.
32% need levothyroxine? that's not a side effect that's a feature
if your body can't handle lithium you shouldn't be on it
stop blaming the drug blame your biology
and for god's sake get your TSH checked before you whine about fatigue
most people just don't want to do the work
you people act like thyroid issues are some minor inconvenience
have you ever had your metabolism die while your brain is still screaming for stability?
levothyroxine doesn't fix the shame of being the person who can't lose weight even when you're eating celery and crying into a salad
and no selenium isn't magic it's just placebo with a price tag
what if the real question isn't whether lithium harms the thyroid
but whether our entire medical system is built on the assumption that we can fix biology with pills without ever asking why the body rebels in the first place
lithium doesn't break the thyroid
it exposes how fragile the system is
and we're not ready to face that
we'd rather adjust the dose than question the premise
hi everyone i just wanted to say i've been on lithium for 11 years and my thyroid is totally fine thanks to yearly blood tests and eating yogurt every morning
also i started taking selenium after reading this and wow it made such a difference in my energy
my doctor was skeptical but i told her i'd rather spend $10 on a supplement than risk crashing into depression again
and honestly if you're worried about your thyroid just ask for free t4 and t3 not just tsh
it's not hard and it saves so much pain
you're not alone in this and there are so many ways to make it work
you deserve to feel like yourself again
people who take lithium and then act like thyroid problems are some tragic accident need to stop acting like victims
you knew the risks when you started
you chose this
now deal with it like an adult
stop demanding everyone else accommodate your biological trade-offs
life isn't fair and neither is psychiatry
get tested get treated stop complaining
i just want to say thank you for writing this
i've been on lithium for 7 years and i thought i was just getting older or that my depression was coming back
when my tsh spiked i felt so alone
but reading this made me feel seen
and i started selenium and my hair stopped falling out in clumps
and i cried because for the first time in years i didn't feel like a broken machine
you're not alone
we're all just trying to stay alive and this post made me feel like maybe i can