
If you’ve been coughing for more than eight weeks, you’re not alone. About 1 in 10 adults in the UK and US deal with a persistent cough that won’t go away. Most of the time, it’s not a cold, flu, or even allergies. It’s something deeper - and often, it’s one of three things: GERD, asthma, or postnasal drip (now called upper airway cough syndrome). The good news? You don’t need endless tests or expensive scans to find out which one it is. A smart, step-by-step approach can get you answers - and relief - in weeks, not years.
What Counts as a Chronic Cough?
A cough that lasts longer than eight weeks is officially called chronic. It’s not just annoying - it can wreck your sleep, make you dizzy, hurt your ribs, or even cause you to leak urine. But here’s the catch: most people assume it’s a lingering infection. It’s not. In fact, only 1-5% of chronic cough cases are caused by bacteria like pertussis (whooping cough). The real culprits are hidden in plain sight - and they don’t always show up on X-rays.
The American College of Chest Physicians laid out the rule in 2006, and it still holds: if you’re not a smoker and you’re not on an ACE inhibitor (like lisinopril or enalapril), then 80-95% of your cough comes from just three sources. That’s why the first step isn’t a CT scan. It’s asking the right questions.
Step One: Rule Out the Red Flags
Before you even think about GERD or asthma, you need to rule out the scary stuff. If your cough comes with any of these, you need urgent evaluation:
- Bloody phlegm (hemoptysis)
- Unexplained weight loss
- Fever that won’t break
- Swelling in your legs or neck
- Clubbing of your fingers (rounded, swollen fingertips)
These aren’t signs of postnasal drip. They could mean lung cancer, tuberculosis, or heart failure. A simple chest X-ray catches most of these. If it’s normal - which it is in 90% of cases - you can move on. No need for a CT scan. The radiation from a single CT equals 74 chest X-rays, and it only finds cancer in about 0.1% of people with normal X-rays and no red flags.
Step Two: Check Your Medications
Did you start a new blood pressure pill in the last six months? If so, that’s probably your cough. ACE inhibitors - drugs like lisinopril, ramipril, and captopril - cause cough in 5-35% of users. It’s not an allergy. It’s a side effect. The cough usually starts within a week to six months after starting the drug. It’s dry, tickly, and worse at night. Stop the pill, and it often clears up in a few days to two weeks. If you’re on one and have a chronic cough, talk to your doctor about switching to an ARB (like losartan or valsartan). They don’t cause cough.
Step Three: The Big Three - GERD, Asthma, Postnasal Drip
Now you’re ready for the core of the workup. These three conditions cause nearly all chronic coughs. But they don’t always act the way you think.
Postnasal Drip (Upper Airway Cough Syndrome)
Most people think of postnasal drip as mucus dripping down the back of the throat. But it’s not just about mucus. It’s about irritation triggering the cough reflex. That’s why the term changed to upper airway cough syndrome - it’s more accurate.
How do you test for it? You don’t need a nasal scope or allergy test. You try treatment. Take a first-generation antihistamine (like chlorpheniramine or diphenhydramine) with a decongestant (pseudoephedrine) for two to three weeks. No nasal spray. No steroid spray. Just the oral combo. If your cough improves by 70-90%, it’s likely UACS.
Response time? Usually 1-2 weeks. If nothing changes after three weeks, move on. Don’t keep taking it. Side effects like drowsiness and dry mouth aren’t worth it if it’s not helping.
Asthma (Cough Variant Asthma)
Most people picture asthma as wheezing and shortness of breath. But in 24-29% of chronic cough cases, cough is the only symptom. That’s called cough variant asthma. No wheeze. No chest tightness. Just a persistent, dry cough - often worse at night, after exercise, or when breathing cold air.
Standard spirometry (lung function test) can be normal in these patients. That’s why a methacholine challenge test is the gold standard. It measures how sensitive your airways are. If your FEV1 drops by 20% or more with a low dose of methacholine, you have airway hyperreactivity - meaning asthma is likely.
Or, you can try a therapeutic trial. Take an inhaled corticosteroid (like fluticasone) for four weeks. If your cough improves by 60-80%, it’s asthma. You don’t need to wait for a challenge test if you’re willing to try treatment. Many doctors skip the test and go straight to the inhaler.
GERD (Gastroesophageal Reflux Disease)
This one’s tricky. Only half the people with GERD-related cough have heartburn. The rest have what’s called silent reflux. The acid doesn’t burn - it irritates the throat and voice box, triggering cough. You might feel a lump in your throat, need to clear your throat constantly, or have a sour taste in your mouth.
Testing for GERD is messy. A 24-hour pH monitor can show reflux, but it’s abnormal in only 50-70% of cough patients. That’s why the standard test is a therapeutic trial. Take a high-dose proton pump inhibitor (PPI) - like omeprazole 40mg or esomeprazole 40mg - twice a day for four to eight weeks. No food two hours before bed. No caffeine, alcohol, or spicy food.
Only 50-75% of people respond. That’s why some experts now say: don’t start PPIs without evidence. But in practice, it’s still the most common first step. If you’re not better after eight weeks, it’s not GERD.
How Do You Know Which One It Is?
Here’s the truth: many people have more than one. A third of patients have both GERD and UACS. Another 20% have asthma and GERD. That’s why the order matters.
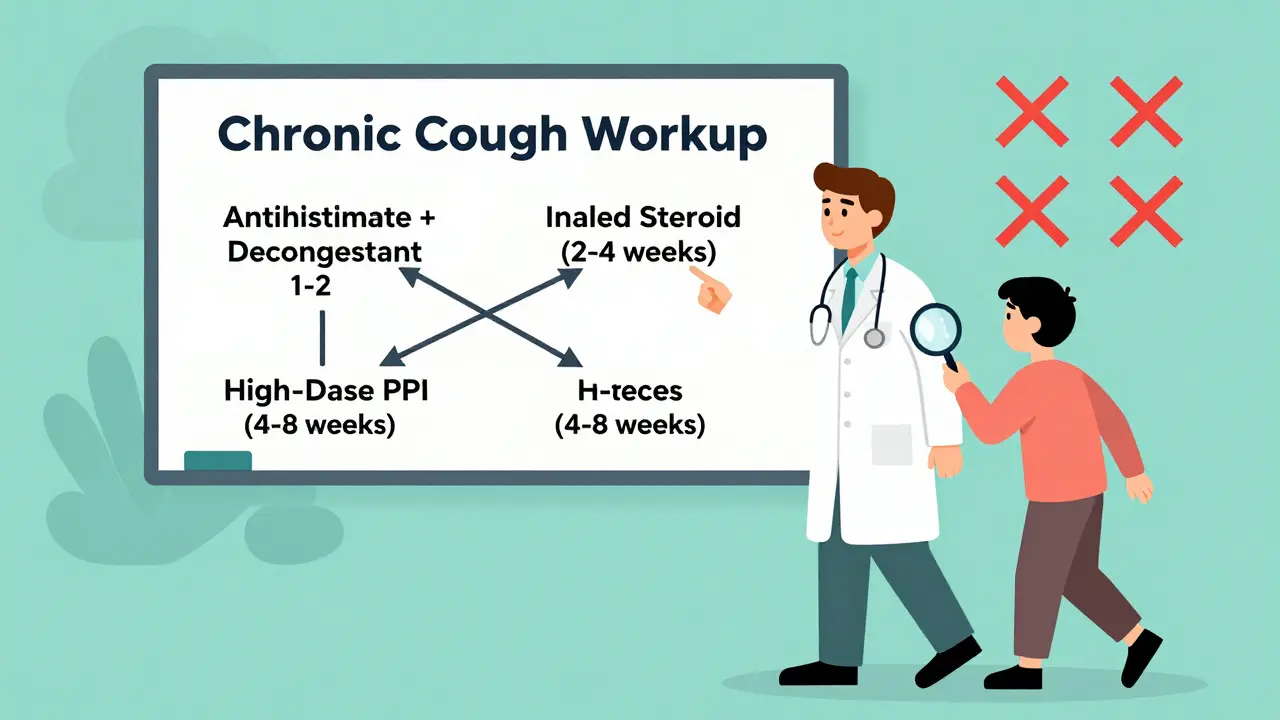
Doctors follow a sequence because some conditions respond faster than others:
- Start with UACS - fastest response (1-2 weeks), easiest to test.
- Then asthma - response in 2-4 weeks, needs inhaler trial or lung test.
- Last, GERD - slowest, 4-8 weeks, and least reliable response rate.
If you’ve tried all three and still cough, you’re in the 10-30% with something else - like chronic refractory cough, vocal cord dysfunction, or even aspiration. But that’s rare. Most people find answers in the first three.
What You Can Do Right Now
You don’t need to wait for a specialist. Here’s your action plan:
- Stop any ACE inhibitor if you’re on one. Ask your doctor for a replacement.
- Take a first-gen antihistamine + decongestant for 14 days. Track your cough daily.
- If no improvement, start an inhaled steroid (like fluticasone) twice daily for four weeks.
- If still coughing, try a high-dose PPI (omeprazole 40mg) twice daily for eight weeks.
- Keep a symptom diary: time of day, triggers, severity. It helps your doctor see patterns.
Don’t take antibiotics. Don’t buy over-the-counter cough syrups - they rarely help chronic cough. And don’t assume it’s allergies. Most allergy meds won’t touch UACS or GERD cough.
Why This Works Better Than Scans
CT scans, bronchoscopies, and allergy tests sound impressive. But they’re not the answer. A 2021 survey of 1,200 UK and US doctors found that 78% of family doctors stick to the three-step trial approach. Only 12% order advanced reflux testing. Why? Because it works.
The Hull Airway Reflux Questionnaire (HARQ) is a free tool you can take online. Score over 13? There’s an 80% chance you have laryngopharyngeal reflux. The Hull Cough Questionnaire scores severity - over 15 means your life is being seriously affected. Use these. They’re validated, free, and better than guessing.
And now, new tools are coming. In 2024, the FDA approved gefapixant for chronic cough - a pill that blocks the cough reflex. Another drug, camlipixant, is under review. These won’t fix the cause - but they’ll help when the cause is hard to find.
What’s Next If Nothing Works?
If you’ve tried all three treatments and still cough, you might have chronic refractory cough (CRC). It’s not in your lungs. It’s in your nerves. Your cough reflex is too sensitive. This isn’t rare - it affects 10-20% of chronic cough patients.
At this point, see a pulmonologist or cough specialist. They may do cough reflex sensitivity testing. They might recommend speech therapy, cognitive behavioral therapy, or newer medications like gefapixant. Don’t give up. There are options - but they start with ruling out the big three first.
Final Thought: Be Patient, But Don’t Wait
Chronic cough isn’t a mystery. It’s a puzzle with three main pieces. Most people find their answer in weeks. But you have to be systematic. Skip the scans. Skip the antibiotics. Start with the evidence-based steps.
If you’ve been coughing for months, you’ve earned relief. You don’t need to suffer through another winter. Start the workup. Track your symptoms. Talk to your doctor. And remember - you’re not crazy. You’re just one step away from answers.






14 Comments
I’ve been coughing for 11 months. Took every pill, did every test. Turns out it was the lisinopril. Switched to losartan. Cough vanished in 9 days. Why do doctors not tell you this first?
Oh my god, I just cried reading this. I thought I was going crazy. My cough kept me awake every night, I was peeing myself laughing, I felt like a broken record. I tried everything-honey, steam, humidifiers, herbal teas. Then I read about the antihistamine + decongestant combo and thought, ‘what do I have to lose?’ Two weeks later, I slept through the night for the first time in a year. This isn’t just medical advice-it’s a lifeline. Thank you for writing this like someone who actually gets it.
Yeah right. ACE inhibitors cause cough? That’s Big Pharma’s cover-up. The real cause is 5G towers messing with your vagus nerve. They don’t want you to know that the cough is your body’s natural defense against electromagnetic poisoning. The PPIs? They’re just suppressing your symptoms so they can sell you more drugs. Read the FDA’s leaked memo from 2019-there’s a whole section on ‘Cough Suppression as Control Mechanism.’ I’ve got screenshots. DM me.
So let me get this straight-you’re telling me I don’t need a $3,000 CT scan to find out why I’m coughing like a dying raccoon? I just gotta stop my blood pressure meds, chug Sudafed, and inhale fluticasone like it’s a vape pen? Bro, that’s the most American thing I’ve ever heard. Also, why does no one talk about how the PPIs make you constipated and feel like your soul’s been vacuumed out? I’m on omeprazole and I swear I’ve aged 10 years. Also, who made up the term ‘silent reflux’? Sounds like a rom-com.
While the pragmatic, stepwise diagnostic approach outlined here is commendable and aligns with current clinical guidelines from the American College of Chest Physicians, it is imperative to emphasize that individual patient variability must be prioritized. The assumption that 80–95% of non-smoker, non-ACE-inhibitor cases are attributable to the triad of UACS, asthma, and GERD may inadvertently delay diagnosis of rarer etiologies such as bronchiectasis, interstitial lung disease, or even early-stage malignancy in at-risk populations. A thorough history and physical examination remain irreplaceable. Furthermore, while therapeutic trials are cost-effective, they should not replace objective diagnostic confirmation where clinical suspicion remains high.
You know, I’ve been thinking about this a lot-not just as a medical thing, but as a metaphor. We live in a world where we’re always chasing symptoms instead of causes. We pop pills for headaches instead of asking why we’re stressed. We take antihistamines for coughs instead of asking why our airways are so hypersensitive. Maybe the real problem isn’t GERD or asthma or postnasal drip-it’s that we’ve forgotten how to listen. To our bodies. To our environments. To the quiet signals we’ve trained ourselves to ignore. This whole ‘trial and error’ approach? It’s not just medicine. It’s mindfulness with a prescription pad.
USA doctors are so lazy they’d rather give you a pill than actually listen. In India, we don’t wait 8 weeks-we go to the ayurvedic doctor, drink ginger-honey-turmeric tea, do jala neti, and pray. Cough gone in 3 days. Why are you wasting time with PPIs and inhalers? You’re not sick-you’re just out of touch with nature. Also, your ‘evidence-based’ approach is just corporate medicine brainwashing you. Wake up.
i just tried the antihistamine thing and it worked?? like i thought it was allergies but nooo it was uacs?? i thought uacs meant i had a runny nose?? wait so its not even about mucus?? i feel dumb now. also i took the ppi and my stomach felt like a rock. why is everything so complicated??
It is deeply concerning that the normalization of therapeutic trials as diagnostic tools has led to the erosion of clinical rigor. While the approach described may yield symptomatic relief in some, it lacks the structural integrity necessary to prevent misdiagnosis. For instance, a patient with early-stage lung cancer may present with a cough and a normal chest X-ray-yet, under this protocol, they would be subjected to an eight-week trial of PPIs, potentially delaying definitive diagnosis. The commodification of medical care has replaced diagnostic precision with convenience. This is not innovation-it is negligence dressed in pragmatism.
USA medical system is a joke. In Russia we just take a shot of vodka and it goes away. Or if it doesn't, you die. Simple. No pills. No tests. No drama. You want to live? Stop coughing. You want to die? Keep taking PPIs. Your choice.
They say GERD causes cough. But what if it’s the other way around? What if the cough is causing the reflux? Like your throat is so irritated it triggers acid to rise? They never talk about that. They just want you to take more pills. I think the whole system is backwards. I’ve been coughing for 3 years. I stopped all meds. Started humming. It’s weird but it works. The vibration calms the nerves. I’m not joking.
Oh, so we’re just supposed to blindly follow this ‘step-by-step’ protocol like obedient little patients? How quaint. I’m sure the pharmaceutical reps who funded this ‘guideline’ are thrilled. You know what’s really behind this? Profit. PPIs make billions. Inhaled corticosteroids? Billions. Antihistamines? Billions. And the ‘cough variant asthma’ diagnosis? Perfect for keeping you on inhalers forever. I’ve seen patients on three different inhalers, two PPIs, and a nasal spray for seven years. Their cough? Still there. Meanwhile, the real issue-diet, stress, air quality-goes unaddressed. You’re not treating the cause. You’re monetizing the symptom.
bro i tried the fluticasone and it made me feel like my throat was full of cotton and my voice sounded like a robot. i stopped. now im on the ppi and my poop is black. is that normal? also why is everyone talking about this like its magic but no one says what happens if you dont get better? what then? do you just die?
It’s fascinating how the medical establishment has turned a neurophysiological phenomenon-chronic cough-into a tripartite diagnostic taxonomy, as if human physiology were a spreadsheet. The reductionism here is almost poetic in its arrogance. We treat the cough as a symptom to be categorized, rather than a signal from a system in distress. The real question isn’t whether it’s GERD or asthma-it’s why the sensory nerves of the larynx have become hypersensitized in the first place. Environmental toxins? Chronic low-grade inflammation? Psychological stress encoded in the vagal tone? These are the questions we refuse to ask because they’re messy, systemic, and don’t come with a branded pill. The ‘stepwise approach’ isn’t medicine-it’s a coping mechanism for clinicians who can’t bear the complexity of the human body.