24 Jan |
12:20 PM

If you have allergies and keep getting sinus infections, you’re not alone. Millions of people with hay fever or environmental allergies deal with constant stuffiness, facial pressure, and thick mucus that won’t clear - even after taking antihistamines. This isn’t just a bad cold that won’t go away. It’s allergy-related sinusitis, a cycle where your immune system overreacts to pollen, dust, or mold, causing your sinuses to swell and trap fluid. And if you don’t break the cycle, it turns into chronic sinusitis - lasting 12 weeks or longer.
Why Allergies Make Sinusitis Worse
Allergies and sinusitis don’t just happen together - they feed each other. When you breathe in an allergen like ragweed or pet dander, your body releases histamine. That makes your nasal passages swell, mucus thickens, and tiny hair-like structures called cilia slow down. Normally, cilia sweep mucus out of your sinuses. When they’re stuck, bacteria and fungi build up. That’s when infection sets in. Studies show that up to 70% of acute sinus infections clear on their own, but for allergy sufferers, that number drops to under 40%. Why? Because the allergen is still in the air. You’re not getting better because you’re still being exposed. It’s like trying to dry your hands while standing under a faucet. And it gets worse. Chronic inflammation from sinusitis can make your nasal lining more sensitive to allergens. So even small amounts of dust or smoke trigger bigger reactions. This creates a loop: allergies → swollen sinuses → infection → more swelling → worse allergies.First-Line Treatments That Actually Work
Forget relying on oral antihistamines alone. They help with sneezing and itchy eyes, but they don’t touch the inflammation deep in your sinuses. The real game-changer? Nasal corticosteroids. Prescription sprays like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce swelling directly at the source. They don’t work overnight - you need to use them daily for 2 to 4 weeks before you feel real relief. But once they kick in, they cut symptoms by about 65%, compared to just 42% for cetirizine (Zyrtec) in head-to-head trials. Here’s the catch: most people stop using them after two weeks because they don’t see instant results. Studies show adherence drops to 35% by week four. That’s why consistency matters more than the brand. Pick one and stick with it.The Power of Saline Irrigation
Nasal rinses aren’t just for old-school remedies. They’re backed by solid science. Using a neti pot or squeeze bottle with a saline solution flushes out allergens, mucus, and irritants. It’s like hitting reset on your nasal passages. The trick is doing it right. Use only distilled water, sterile water, or water boiled for at least one minute and cooled. Tap water can carry dangerous microbes like Naegleria fowleri - rare, but deadly. Mix one packet of saline (available at pharmacies) with 240ml of safe water. Tilt your head sideways over the sink, let the solution flow through one nostril and out the other. Do this once or twice a day, especially after being outdoors. People who rinse daily report fewer sinus infections, less need for antibiotics, and better sleep. It’s cheap, safe, and works better than most over-the-counter decongestants.When Antibiotics Help - and When They Don’t
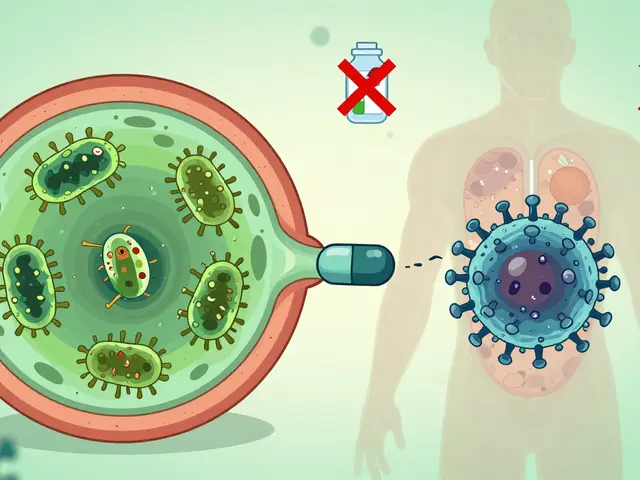
Antibiotics are often prescribed for sinusitis, but they’re only useful if bacteria are involved. In pure allergy-driven cases, they’re useless. In fact, research shows antibiotics work in only 35-45% of allergy-related sinusitis cases, compared to 78-87% in straightforward bacterial infections. So when do you need them? If symptoms last more than 10 days, get worse after initial improvement, or include high fever, thick yellow-green mucus, or severe facial pain, then a bacterial superinfection is likely. First-line treatment is amoxicillin 500mg three times a day for 5-10 days. If you’ve had recent antibiotics or your symptoms are severe, your doctor might prescribe amoxicillin-clavulanate (Augmentin) at 2g twice daily. Don’t push for antibiotics if you’ve only been sick for a week. Overuse leads to resistant bacteria and makes future infections harder to treat.
Biologics: The New Hope for Severe Cases
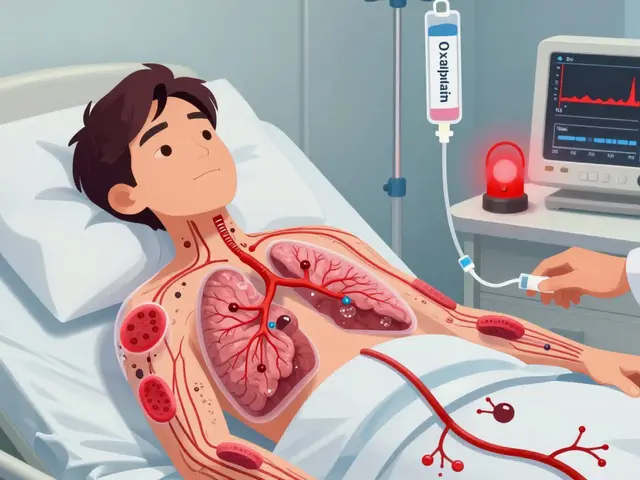
If you’ve tried everything - steroids, rinses, antibiotics - and still have nasal polyps, blocked sinuses, or constant pressure, it’s time to talk about biologics. These are injectable medications that target specific parts of the immune system driving inflammation. Dupilumab (Dupixent) blocks interleukin-4 and -13, two key proteins in allergic inflammation. In trials, it reduced nasal polyp size by 73% and improved breathing in over 80% of patients. Omalizumab (Xolair) and mepolizumab (Nucala) are also approved for this use. Tezepelumab (Tezspire), approved in early 2023, shows promise for patients who didn’t respond to other biologics. But here’s the reality: these drugs cost around $3,500 a month without insurance. Most patients need prior authorization, and coverage varies. Still, for those with severe, uncontrolled sinusitis and polyps, they can be life-changing - reducing the need for surgery and improving quality of life dramatically.Immunotherapy: Breaking the Cycle for Good
If you know your triggers - whether it’s pollen, dust mites, or cat dander - allergy shots (subcutaneous immunotherapy) can change your long-term prognosis. Unlike meds that mask symptoms, immunotherapy retrains your immune system to stop overreacting. It starts with weekly injections for 4-6 months, then monthly shots for 3-5 years. The payoff? 60-70% of patients see a major drop in sinus infections after completing treatment. That’s far better than the 25-30% improvement you get from meds alone. Allergy testing - either skin prick or blood tests - is the first step. If you’re allergic to multiple things, or if your environment is hard to control (like living in a city with high pollution), immunotherapy becomes even more valuable.When to See an ENT Specialist
You don’t need to suffer for months before getting help. See an ear, nose, and throat (ENT) doctor if:- Your symptoms haven’t improved after 4-6 weeks of proper nasal steroid use and daily rinses
- You have nasal polyps (visible in the nose or confirmed on scan)
- You’ve had four or more sinus infections in a year
- You feel pressure around your eyes, headaches that worsen when bending over, or vision changes
- You have a history of asthma or aspirin sensitivity - these are red flags for more complex conditions like AERD (aspirin-exacerbated respiratory disease)



9 Comments
Been using saline rinses for 6 months now and honestly? My sinuses haven’t felt this clear since college. No more 3am nose-blowing marathons.
Yo I just wanna say this post is straight fire. I used to think nasal sprays were for old people with sniffles, but after 3 weeks of fluticasone daily? My face stopped feeling like a water balloon during pollen season. And the saline rinse? I do it while watching Netflix now - weird but worth it. I didn’t know my sinuses could feel this light. Like my head finally stopped carrying a backpack full of wet socks. If you’re on the fence, just start with the rinse. No meds, no cost, no drama. Your nose will thank you. And if you’re like me and forget to use the spray? Set a damn alarm. I use one called ‘Don’t Be a Snotty Ghost’.
Wow, so let me get this straight - you’re telling me I’m supposed to spend $3,500 a month on an injection just so I can breathe? And the government won’t cover it? Meanwhile, my cousin’s cousin’s dog got a $20,000 vet bill for ‘emotional support acupuncture’ and insurance paid for it. This system is a joke. I’d rather just live in a plastic bubble than pay for biologics. Also, who says allergies are real? Maybe it’s just stress. Or bad vibes. Or the fact that we’re all just too soft now. I haven’t used a tissue in 8 years. I just sniff. Hard. And it works.
bro i tried the neti pot and i think i almost died. water went in my ear and i heard a gurgle like a swamp monster. now i’m scared to even sneeze. why is this so hard? i just want to be normal again. also can i just take benadryl forever? it makes me sleepy but at least i don’t feel like my skull is cracking.
Thank you for writing this with such care. I’ve struggled with this for over a decade and felt so alone. Your explanation of the cycle - allergies → swelling → infection → more swelling - finally made sense to me. I started rinses last month and already feel lighter. Not cured, but hopeful. That’s more than I’ve had in years. You’re not just sharing info - you’re giving people back their breath.
Okay but let’s be real - this whole post reads like a pharmaceutical ad disguised as a public service announcement. Who even is this guy? Is he getting paid by GlaxoSmithKline to push Flonase? I’ve been using saline rinses since 2012 and guess what? I still get sinus infections. Because the real problem isn’t the mucus - it’s the fact that we’re all breathing in chemical soup from air conditioning units, industrial farming, and glyphosate-laced pollen. And don’t get me started on how the ENT industry profits off polyp removals like it’s a franchise. Biologics? Sure, let’s inject $3,500/month of monoclonal antibodies into people who can’t afford rent. Meanwhile, the EPA ignores mold in public housing and calls it ‘allergies’. This isn’t medicine - it’s capitalism with a stethoscope. And don’t even get me started on immunotherapy. Three years of needles? That’s not a cure - that’s a cult. I’d rather live with a blocked nose than become a walking lab rat for Big Pharma’s latest profit scheme.
One must pause and reflect upon the metaphysical implications of nasal mucosal dysregulation within the context of late-stage anthropocene immunological collapse. The sinuses, those sacred caverns of pneumatic sovereignty, have become the battleground where the individual’s Aristotelian essence is besieged by the Hegelian dialectic of environmental toxins and corporate pharmacology. To prescribe fluticasone is not merely to suppress inflammation - it is to acquiesce to a techno-bureaucratic regime that pathologizes natural biological variance. Yet, paradoxically, to eschew treatment is to surrender one’s pneumatic autonomy to the whims of airborne allergens - themselves manifestations of industrial hubris. Thus, we are caught in an ontological quandary: to heal is to submit; to resist is to suffer. The solution? Perhaps not in syringes or sprays, but in the quiet reclamation of ancestral breath - through nasal breathing, through fasting from processed air, through the sacred ritual of silence beneath a canopy of native oaks. Alas, few possess the fortitude for such a path.
So let me get this straight - you’re telling me the cure for my sinusitis is… to pay $3,500 a month and pray to the gods of insurance? Meanwhile, my grandma used to rub Vicks on her chest and say a prayer to St. Jude. She lived to 98. I think we lost our way somewhere between the neti pot and the biologic drip. Also, why does every medical article now sound like a TED Talk written by a grad student on Adderall? Just tell me what to do, not how it ‘retrains the immune system’. I just want to sleep without sounding like a foghorn.
omg i just read this whole thing and i’m crying?? i’ve had this for 12 years and felt so guilty for being ‘dramatic’ about it. my husband thinks i’m just whining but this? this is exactly what’s happening. i started rinses last week and already my eyes don’t feel like they’re glued shut. i’m gonna try the steroid spray too. i’m so tired of being tired. thank you thank you thank you. also i just typed ‘steriod’ instead of ‘steroid’ and i’m not even sorry. this is my emotional breakthrough post.