
Skipping a pill here and there might seem harmless. Maybe you forgot. Maybe you felt fine. Maybe the cost was too high. But when you don’t take your medication exactly as your doctor ordered, the consequences aren’t just theoretical-they’re life-altering, and often deadly.
Every Missed Dose Adds Up
You might think missing one dose won’t matter. But medication works best when it’s in your system at consistent levels. Antibiotics? If you stop early, the surviving bacteria come back stronger. Blood pressure pills? Skipping them lets your pressure spike, damaging arteries you can’t even feel. Diabetes meds? A single skipped insulin shot can send blood sugar soaring, leading to hospital visits or worse.Studies show that for chronic conditions like high blood pressure, heart failure, or asthma, adherence rates hover around 50%. That means half the people taking these drugs aren’t taking them right. And it’s not because they’re careless-it’s because the system isn’t built to help them succeed.
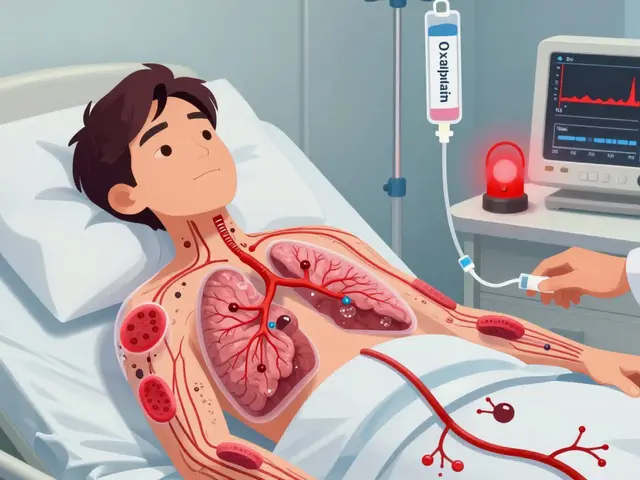
Death Is a Real Risk
Nonadherence kills. Not in dramatic headlines, but quietly, every day. In the U.S. alone, it’s linked to about 125,000 preventable deaths each year. That’s more than traffic accidents. For people over 50, the risk of dying from skipping meds is up to 30 times higher than the risk of being murdered.Organ transplant patients who miss anti-rejection drugs risk losing their new organs. Heart patients who skip statins or beta-blockers are far more likely to have heart attacks. Diabetics who skip insulin face diabetic ketoacidosis-a condition that can kill within hours if untreated. And for those with mental health conditions like schizophrenia or bipolar disorder, skipping medication increases the chance of crisis, hospitalization, or suicide.
It Costs You-and Everyone Else-Big Time
When you don’t take your meds, the hospital bill doesn’t just land on you. It lands on the whole system. In 2016, medication nonadherence cost the U.S. healthcare system an estimated $529 billion. That’s not a typo. That’s half a trillion dollars.Why? Because skipped doses lead to complications. Complications lead to ER visits. ER visits lead to hospital stays. And 20% of Medicare readmissions within 30 days are directly tied to patients not taking their meds. Each avoidable hospitalization can cost $10,000 to $50,000. Multiply that by millions of people, and you get the staggering total.
And it’s not just hospitals. Missed work, lost productivity, caregiving burdens-all add up. In the EU, nonadherence creates €80-125 billion in avoidable costs annually. That’s money that could go to schools, roads, or better care.

Cost Is the Biggest Barrier
Let’s be real: if your prescription costs $200 a month and you’re choosing between medicine and groceries, you’re not being irresponsible-you’re surviving.According to the CDC, 8.2% of adults aged 18-64 admitted they didn’t take their medication as prescribed because they couldn’t afford it. That number is rising. Out-of-pocket drug spending jumped 4.8% in 2021 alone. For older adults on fixed incomes, or young people working hourly jobs without insurance, this isn’t a choice-it’s a trap.
And it’s worse for Black, Latino, and other minority communities. Historical distrust, language barriers, pharmacy deserts, and systemic gaps in care make adherence even harder. These aren’t personal failures-they’re failures of the system.
Complex Regimens Break People
Taking five different pills at three different times a day? With food? Without food? With water? Without caffeine? It’s no wonder people give up.Many patients are handed a thick packet of pills with no clear explanation. No one sits down and says, “Here’s why each one matters.” They’re left guessing. And when side effects show up-dizziness, nausea, fatigue-they assume it’s normal. They don’t tell their doctor. They just stop.
One study found that adherence drops sharply after the first few months. The initial motivation fades. The reminders stop. The confusion grows. And by six months, nearly half are no longer taking their meds correctly.

What Actually Works to Fix This
It’s not about shaming people. It’s about removing barriers.Pharmacists who check in with patients-just once a month-can boost adherence by 15-20%. Simple text message reminders improve it by 12-18%. Pill organizers with alarms? They help. Medication therapy management programs-where a pharmacist reviews your entire list of drugs-save money and lives.
Some clinics now bundle pharmacy and medical care. Instead of seeing your doctor and then going to a separate pharmacy, you get both under one roof. That cuts confusion, reduces travel, and builds trust. And it works-especially for people who’ve been failed by the system before.
Technology is helping too. AI tools can now predict who’s at risk of skipping meds-with 70-85% accuracy-so providers can step in before a crisis hits. But none of this matters if insurance won’t pay for it. Right now, most adherence programs aren’t reimbursed. So clinics don’t offer them. And patients suffer.
You’re Not Alone-But You Have to Speak Up
If you’re skipping doses because of cost, side effects, or confusion, you’re not lazy. You’re not failing. You’re responding to a system that doesn’t work for you.But you can change that. Tell your doctor. Tell your pharmacist. Say: “This is too expensive.” “I don’t understand why I need this.” “I’m having bad side effects.”
There are often alternatives. Generic versions. Lower-dose options. Assistance programs. Mail-order pharmacies. Even switching to a once-daily pill instead of three.
And if your provider brushes you off? Find another. Your life isn’t a footnote in a chart. It’s the whole point.
It’s Not Just About Pills-It’s About Trust
The real problem isn’t just forgetfulness or cost. It’s broken trust. Too many people have been burned-by dismissive doctors, by surprise bills, by being told their symptoms are “all in their head.”Adherence isn’t about compliance. It’s about partnership. When your provider listens, explains, and works with you-not just at you-you’re far more likely to stick with the plan.
That’s the shift we need: from blaming patients to fixing systems. From seeing nonadherence as a personal failure to recognizing it as a public health emergency.
Because every time someone skips a pill, it’s not just their body that pays the price. It’s their family. Their community. Their future.


11 Comments
People just don’t get it. Skipping meds isn’t some little white lie it’s a slow-motion suicide pact with your own body. You think you’re saving cash but you’re just setting up your family for a funeral they didn’t sign up for. I’ve seen it. My uncle skipped his blood pressure pills for months because he "felt fine." Then one morning he dropped dead in the driveway. No warning. No drama. Just gone. That’s not tragedy. That’s negligence dressed up as independence.
My grandma used to take all her meds like clockwork. Every single day. Even when she was in pain or tired. She said "If the doctor gave it to me, it’s for a reason." And she was right. I used to roll my eyes until I saw her get sick after forgetting her diuretics. Took three days in the hospital. One pill. Three days. That’s the math. Don’t be the person who makes the system pay for your forgetfulness.
Let’s be real here. This whole article is just another liberal guilt trip wrapped in medical jargon. You want people to take their pills? Fix the damn system. Make drugs cheap. Stop letting Big Pharma gouge people. Blaming the sick for being poor is the oldest trick in the book. And no, I’m not some conspiracy nut. I’m just tired of people pretending poverty is a moral failing.
my mate got his insulin cut in half cause he couldnt afford it. then he ended up in a coma for 2 weeks. hospital bill was 80k. insurance paid 50k. the rest? taxpayer. so yeah. skip your meds. let the rest of us foot the bill. real responsible. 😑
wait so if someone skips a pill because they cant afford it, is that technically nonadherence? or is that a system failure? i feel like the article blames the person but the real problem is the cost. like… if you told me i had to choose between my meds and my kid’s school lunch, i’d skip the meds too. no shame in that.
Discipline isn’t optional. Your health is your #1 asset. If you can’t manage five pills a day, you’re not broken-you’re untrained. Start small. Use alarms. Get a pillbox. Track it. Build the habit like you’re building muscle. No one’s coming to save you. But you can save yourself.
Look. The entire pharmacological industrial complex is a performative charade masquerading as science. We’re not treating disease-we’re monetizing dependency. The system doesn’t want you healed. It wants you compliant. And the real tragedy isn’t the missed doses-it’s that we’ve internalized the lie that your worth is measured by your adherence to corporate-prescribed biochemistry. You’re not a patient. You’re a revenue stream with a pulse. And the moment you start seeing that, you’ll understand why people stop taking the pills. Not because they’re lazy. Because they’re awake.
While the emotional weight of this piece is undeniable, I must emphasize the global perspective. In nations with universal healthcare, adherence rates exceed 80%. The issue is not cultural laziness-it is structural. The U.S. model, which externalizes cost onto individuals, is fundamentally incompatible with chronic disease management. Policy reform, not personal admonishment, is the only sustainable solution.
For anyone struggling: ask your pharmacist about patient assistance programs. Most drug makers have them. Some pills are free if you qualify. Also-tell your doctor about side effects. There’s always another option. I’ve helped people switch from 4 pills a day to 1. It’s not magic. It’s just talking.
you’re not alone. i know it feels like everyone else has it together but they don’t. even the ones who seem perfect. just say one thing to your dr. "this is too hard." that’s all it takes to start changing things.
They’re using your meds to track you. The pills have microchips. The system knows who skips. They flag you for surveillance. Next thing you know, your benefits get cut, your car gets repossessed, your kid gets taken. This isn’t about health. It’s about control. You think you’re choosing between food and pills? No. You’re choosing between survival and being erased.