Uterine Health: Simple, Practical Steps to Stay on Top of It
Uterine health touches periods, pregnancy, and daily comfort. If something feels off — heavy bleeding, bad pain, odd discharge — don't ignore it. Small changes can point to common issues like fibroids, endometriosis, polyps, or infections. This page explains what to watch for, which tests help, and clear next steps you can take.
Signs worth tracking: how long your period lasts, how much you bleed, pain level, and any unusual discharge or smell. Keep a short log on your phone. Heavy bleeding means soaking more than one pad or tampon an hour for several hours, or needing double protection. Severe, sudden pain that stops you from normal activity or causes fainting needs urgent care.
Common uterine problems in plain language
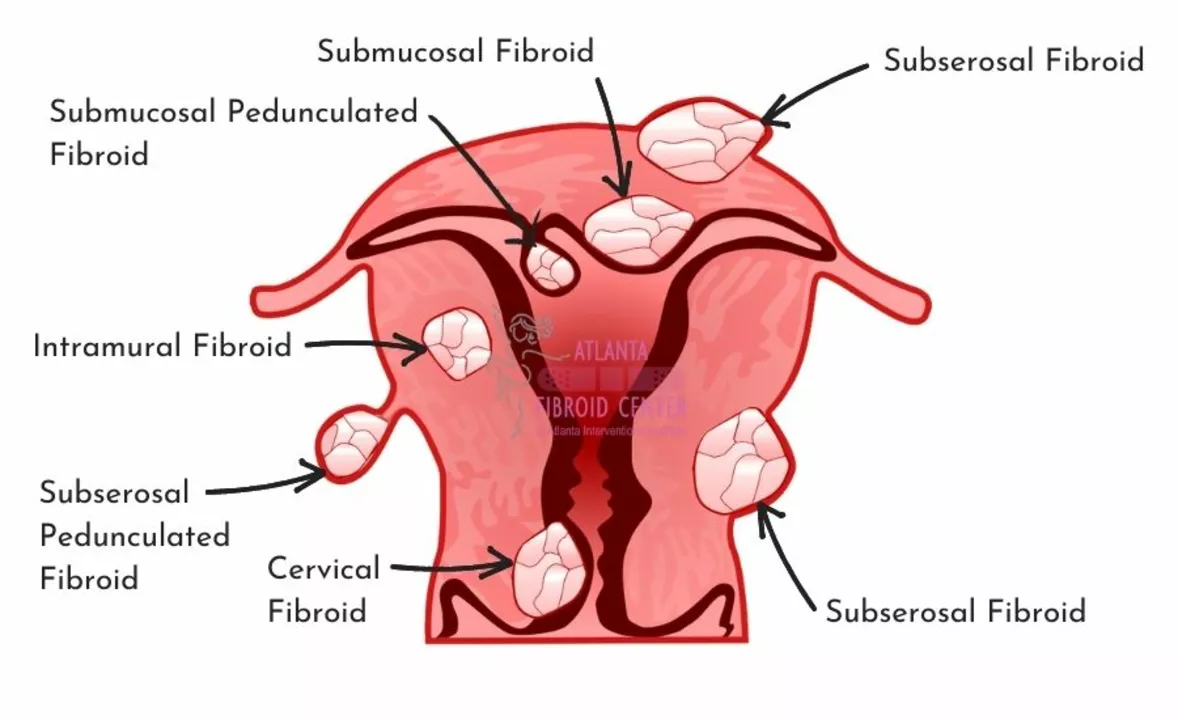
Fibroids — noncancerous growths that can cause heavy periods, pelvic pressure, and frequent urination. Many people live with fibroids and need only monitoring; others need medication or a procedure.
Endometriosis — tissue like the lining of the uterus grows outside it. Expect painful periods, pain during sex, and sometimes fertility issues. Symptoms are often worse than regular cramps and don’t always match what you see on scans.
Polyps and adenomyosis — small growths or tissue changes inside the uterus that can cause irregular bleeding or pain. Infections (like PID) cause fever, bad-smelling discharge, and pelvic pain — treatable with antibiotics.
Tests and quick fixes that actually help
Start with a pelvic exam and talk about your period log. A transvaginal ultrasound is the usual first imaging test — it shows fibroids, polyps, and lining thickness. If bleeding is abnormal, an endometrial biopsy or hysteroscopy may be recommended to check the uterine lining. Blood tests (CBC) can check for anemia if you’re losing a lot of blood.
For symptom relief: NSAIDs (ibuprofen) help period pain and reduce bleeding for many people. Tranexamic acid cuts heavy bleeding for those without contraindications. Hormonal options — combined birth control pills, progestin-only pills, or a hormonal IUD (levonorgestrel) — can reduce bleeding and pain and sometimes shrink fibroids. For infections, follow the prescribed antibiotic course fully.
Surgery is not the first step for most. Minimally invasive options like hysteroscopic removal of polyps or myomectomy for targeted fibroid removal keep fertility options open. Hysterectomy is a definitive fix but comes with long-term consequences; discuss fertility, hormones, and recovery before deciding.
Simple lifestyle moves help: keep a healthy weight, manage diabetes or high blood pressure, quit smoking, and eat iron-rich foods if you’re anemic. Regular checkups and screening tests per your doctor’s advice catch many problems early.
If you have heavy bleeding, fever with pelvic pain, fainting, or sudden severe pain, seek care now. For ongoing symptoms, make an appointment with a gynecologist who listens and offers clear options. Your uterus deserves straight talk and practical care — and you deserve to feel normal again.
How Overgrowth in the Lining of the Uterus Can Lead to Abnormal Bleeding
As a blogger, I've recently been researching how overgrowth in the lining of the uterus can lead to abnormal bleeding. I discovered that this overgrowth, known as endometrial hyperplasia, can cause the uterine lining to become too thick, resulting in heavy or prolonged periods. Additionally, hormonal imbalances, such as elevated levels of estrogen without enough progesterone, can contribute to this condition. It's important to consult with a healthcare professional if you're experiencing abnormal bleeding, as it could be a sign of an underlying issue. Early detection and treatment can help prevent more severe complications, such as infertility or even cancer.
view more




