Gut Bacteria: How Your Microbiome Affects Health, Medications, and Daily Wellness
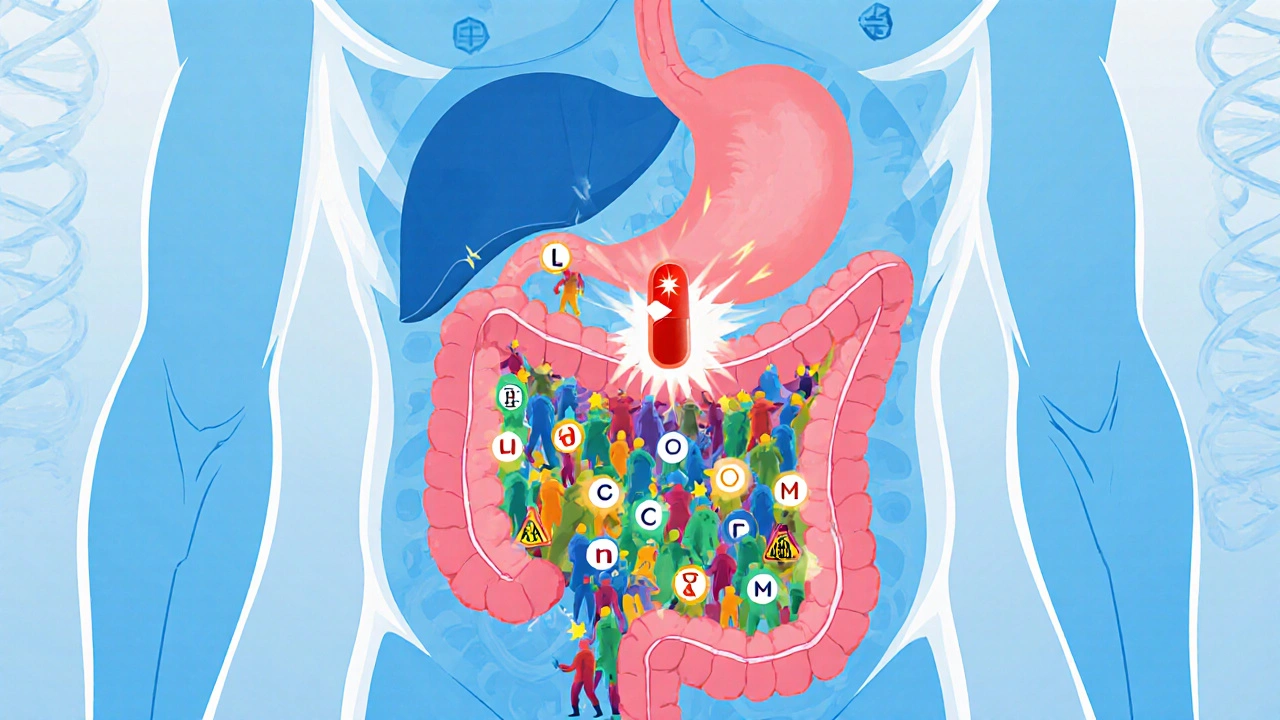
When you think about your health, you probably focus on your heart, lungs, or blood pressure. But the real powerhouse living inside you? Your gut bacteria, trillions of microorganisms living in your digestive tract that help break down food, train your immune system, and even influence your mood. Also known as your microbiome, this invisible ecosystem is as unique as your fingerprint—and it’s directly tied to how your body responds to medications, supplements, and even stress.
Here’s the thing: gut bacteria don’t just sit around digesting your lunch. They interact with nearly every drug you take. Antibiotics? They wipe out good and bad bugs alike, sometimes causing diarrhea or yeast infections. Probiotics? They can help rebuild what’s lost—but not all strains work the same. Even common meds like antidepressants, painkillers, and cholesterol drugs are affected by what’s going on in your gut. Studies show that people with different gut bacteria profiles respond differently to the same pill. That’s why two people taking the same dose of a drug might have totally different side effects—or none at all.
Your gut bacteria also play a role in inflammation, which links to heart disease, diabetes, and even joint pain. That’s why you’ll see posts here about bempedoic acid, a cholesterol drug linked to gout and tendon risks, and how gut health might influence those reactions. Or why diabetes, a condition that damages blood vessels and nerves, is tied to changes in microbial balance. Even heart failure, a condition where the heart can’t pump efficiently, has been connected to gut-derived toxins that leak into the bloodstream when the microbiome is out of balance. This isn’t theory—it’s clinical observation backed by growing research.
What you eat, how much you sleep, whether you’re stressed, and even how often you take antibiotics all shift your gut bacteria. That’s why managing your microbiome isn’t just about popping probiotics—it’s about lifestyle. Some people find relief from bloating or fatigue just by switching fiber sources. Others notice fewer side effects from meds after adjusting their diet. And yes, some supplements marketed for gut health? They don’t work. Others? They can make a real difference—if you pick the right ones.
In the posts below, you’ll find real-world guides on how gut bacteria connect to medications you’re already taking. From how antibiotics trigger yeast overgrowth to why some people get gout after taking cholesterol drugs, these aren’t abstract ideas—they’re practical insights from people managing real conditions. You’ll learn what to watch for, what to ask your doctor, and what actually helps your gut stay balanced. No fluff. No hype. Just clear, actionable info that ties your daily choices to what’s happening inside you.
How Your Gut Bacteria Affect Drug Side Effects and Effectiveness
Your gut bacteria can turn medications into toxins or make them useless. Learn how microbiome-drug interactions cause unexpected side effects and what’s being done to personalize treatment.
view more




