Gastrointestinal health: what to watch for and what actually helps
Stomach pain, heartburn, constipation or diarrhea — these complaints are common, but they don’t have to rule your life. This page gives clear, usable steps you can try today, explains when symptoms need a doctor, and points to reliable reads on specific meds like pantoprazole and sulfasalazine.
Quick fixes and daily habits that make a real difference
Start with food and timing. Avoid large meals late at night, cut back on fried, spicy, and highly acidic foods if you get reflux, and eat slowly. For constipation, add fiber gradually (oats, beans, fruit) and drink more water — sudden big increases in fiber can actually make things worse at first.
Move more. Walking after meals helps digestion and lowers reflux episodes. If you’re overweight, even 5–10% weight loss often reduces heartburn and improves overall gut symptoms.
Sleep smarter. Raising the head of the bed a few inches or using a wedge pillow keeps stomach acid down at night. Avoid lying flat within two hours after eating.
Think about what you drink. Cut or limit alcohol, coffee, and fizzy drinks if they trigger your symptoms. Plain water or herbal tea usually causes fewer problems.
When to see a doctor and medication basics
See a clinician fast if you have severe belly pain, unexplained weight loss, blood in stool or vomit, persistent vomiting, or new difficulty swallowing. These are not normal and need evaluation.
Medications can help but they each have pros and cons. Proton pump inhibitors (PPIs) like pantoprazole are very effective for reflux and ulcers — learn practical tips on use and side effects in our Protonix guide: Protonix (pantoprazole). For inflammatory bowel conditions, sulfasalazine (Azulfidine) and short steroid courses (like prednisone/Deltasone) are used differently — read about benefits and risks before adjusting treatment: Azulfidine, Deltasone (prednisone).
Antibiotics can cause diarrhea or yeast overgrowth. If a recent antibiotic course lines up with new symptoms, check the amoxicillin advice and talk to your doctor: Amoxicillin dosage for children (notes apply to adults too).
Small tests often help: stool checks, basic bloods, endoscopy for persistent issues. For suspected parasites, targeted testing matters — our piece on parasite evolution explains why one-size-fits-all treatment isn’t smart: Parasite infections and treatments.
Final practical tip: keep a short symptom diary — what you ate, sleep, stress, and medication — for two weeks before a clinic visit. It makes diagnosis faster and keeps you from guessing. If you want, explore the linked guides above to learn about specific drugs and safe online options for prescriptions.
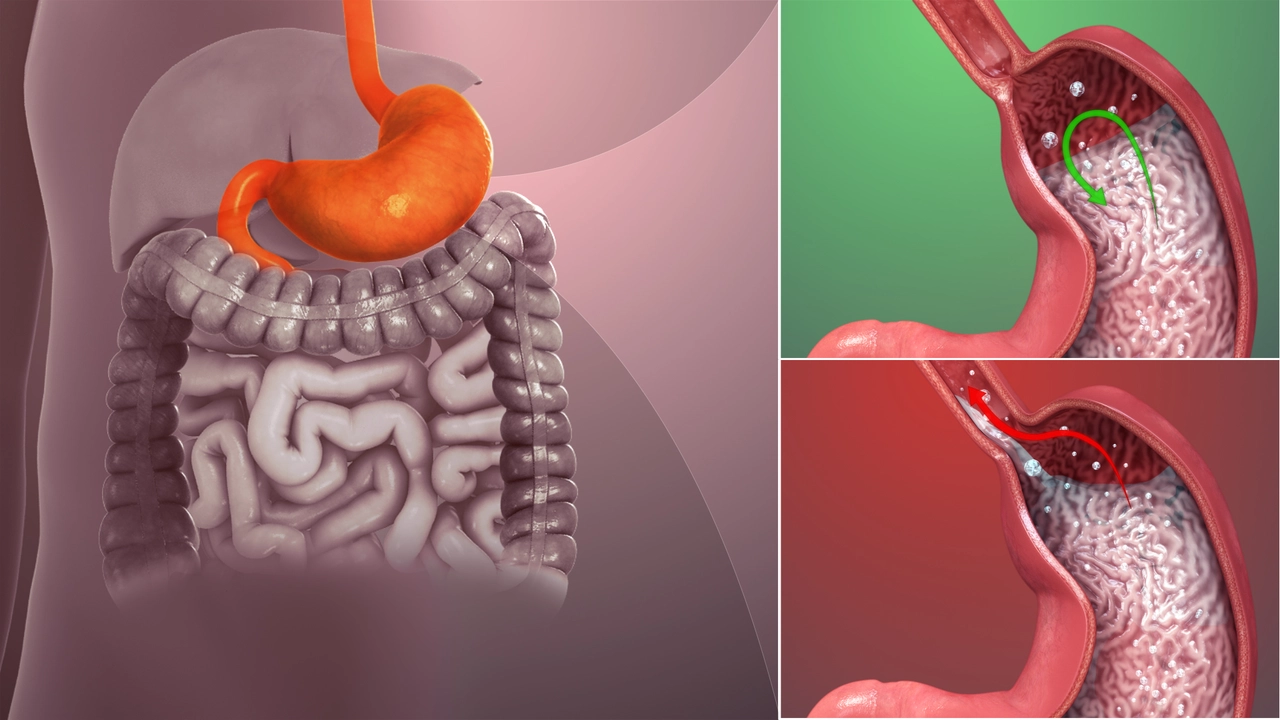
The Connection Between Acid Reflux and Erosive Esophagitis
In my latest research, I delved into the strong link between acid reflux and erosive esophagitis. Acid reflux, also known as GERD, is a condition where stomach acid flows back into the esophagus, which can cause inflammation and damage, leading to erosive esophagitis. Essentially, repeated instances of acid reflux can cause the lining of the esophagus to erode, causing discomfort and potentially serious health issues. It's crucial to manage acid reflux symptoms to prevent this escalation. Overall, understanding the connection between these two conditions is key for effective treatment and management.
view more




