Understanding Acid Reflux and Erosive Esophagitis
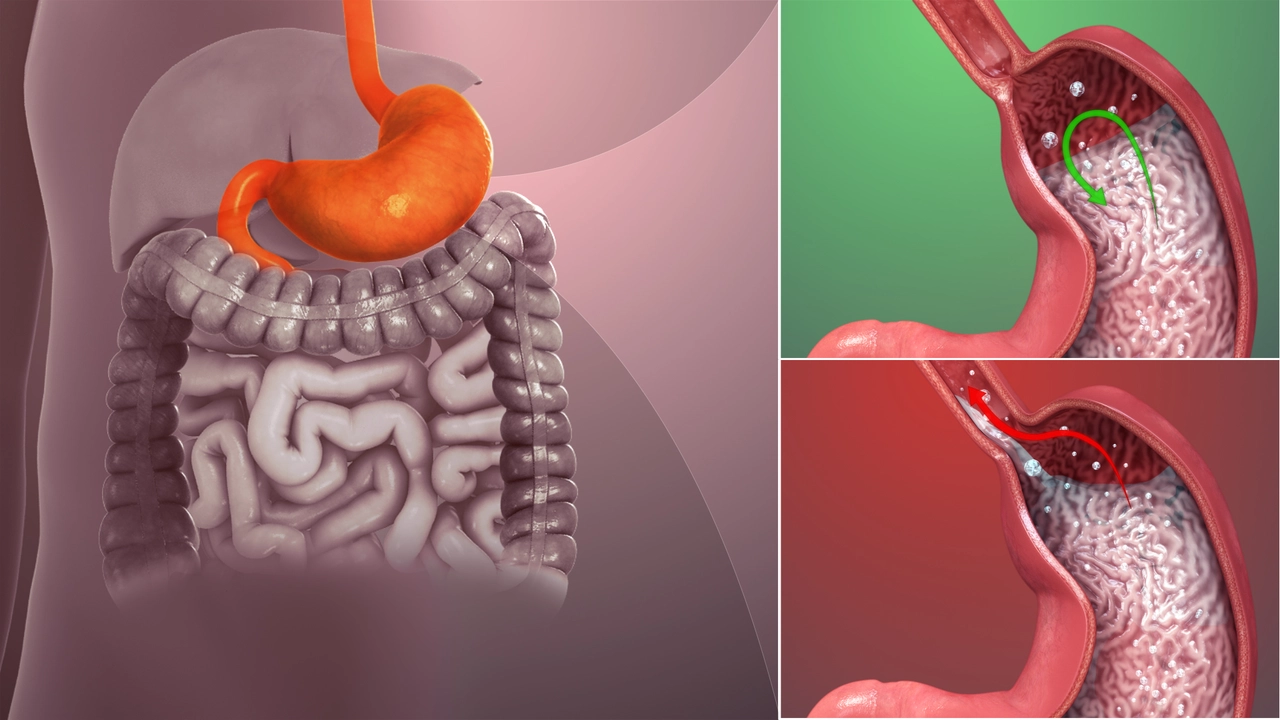
Before diving into the connection between acid reflux and erosive esophagitis, let's take a moment to understand what each of these conditions are. Acid reflux, also known as gastroesophageal reflux disease (GERD), is a condition where stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of your esophagus, causing discomfort and even damage over time.
Erosive esophagitis, on the other hand, is an inflammation of the esophagus that's often caused by GERD. It occurs when the protective lining of the esophagus becomes damaged, leading to inflammation and ulcers.
The Link Between Acid Reflux and Erosive Esophagitis
Now, you might be wondering, what exactly is the connection between these two conditions? Well, the answer is pretty straightforward. The persistent backwash of stomach acid that characterizes acid reflux can damage the lining of the esophagus. Over time, this damage can lead to inflammation and ulcers, which are the hallmarks of erosive esophagitis. So, in essence, acid reflux, if left untreated, can lead to erosive esophagitis.
Signs and Symptoms of Acid Reflux and Erosive Esophagitis
Knowing the signs and symptoms of both acid reflux and erosive esophagitis can help you seek treatment early and potentially prevent long-term damage to your esophagus. Common signs of acid reflux include heartburn, regurgitation of food or sour liquid, and difficulty swallowing. On the other hand, symptoms of erosive esophagitis might include chest pain, difficulty swallowing, and in severe cases, bleeding from the esophagus.
Diagnosing Acid Reflux and Erosive Esophagitis
Diagnosis for these conditions usually begins with a thorough physical examination and a review of your medical history. Your doctor may also recommend certain tests such as an endoscopy to examine your esophagus and stomach, a biopsy to check for inflammation or Barrett's esophagus, or a pH monitoring to measure acid in your esophagus.
Treatment Options for Acid Reflux and Erosive Esophagitis
There are various treatment options available for acid reflux and erosive esophagitis. These include lifestyle changes like avoiding foods that trigger heartburn, losing weight if you're overweight, and quitting smoking. Medications may also be prescribed to reduce stomach acid and promote healing. In severe cases, surgery might be considered to strengthen the lower esophageal sphincter.
Complications of Untreated Acid Reflux and Erosive Esophagitis
If left untreated, acid reflux and erosive esophagitis can lead to serious complications. These may include narrowing of the esophagus, open sores or ulcers in the esophagus, and a precancerous condition called Barrett's esophagus. It's important to seek treatment if you're experiencing symptoms of these conditions.
Preventing Acid Reflux and Erosive Esophagitis
Prevention is always better than cure. Making certain lifestyle changes can go a long way in preventing acid reflux and erosive esophagitis. These include maintaining a healthy weight, avoiding foods that trigger heartburn, not lying down soon after meals, and quitting smoking. Regular check-ups with your doctor can also help detect any early signs of these conditions.






15 Comments
If you think acid reflux is just a minor inconvenience, you’re buying the lie sold by the snack industry. The relentless backwash of stomach acid is tearing down the esophageal lining faster than a demolition crew on a budget. Ignoring the warning signs only guarantees you’ll end up with erosive esophagitis, a condition no one wants to brag about. Wake up, America, and start taking this seriously.
Choosing to ignore the warning signs of reflux is tantamount to self‑sabotage. Every time you light up a cigarette or gorge on greasy take‑out you’re signing a death warrant for your own esophagus. It’s a moral duty to your future self to ditch those habits before the damage becomes irreversible. The only thing you’re protecting is your dignity.
yeah the whole reflux thing is kinda annoying but the key is just not lying down after meals it really does help and cutting back on the spicy stuff can make a big difference
Oh wow, another deep dive into the thrilling world of stomach acid, how could anyone possibly stay awake reading this?
Let’s be honest, most people only notice reflux when the burning sensation ruins their favorite midnight pizza.
And then there’s the classic "heartburn" that feels like a tiny dragon doing flamethrowers in your chest, right?
Seriously, if you’re still wondering why your throat feels like sandpaper, maybe stop treating your body like a rain‑gutter.
Complex medical jargon can be intimidating, but the core idea is simple: acid loves to party, and your esophagus is the uninvited guest.
Skipping a meal? Bad idea. Binge‑eating a pizza? Double bad.
Elevating the head of your bed by a few inches is a low‑effort hack that actually works.
And no, drinking a glass of water right after a heavy meal won’t neutralize the acid – it might just push it further down.
People often think medication is a magic bullet, but lifestyle changes are the real MVPs.
Weight loss can reduce abdominal pressure, meaning less acid gets forced upward.
Quitting smoking isn’t just about lungs; the nicotine relaxes the lower esophageal sphincter, making reflux easier.
If you’re experiencing bleeding, that’s a red flag screaming louder than a bullhorn – see a doctor ASAP.
Endoscopy isn’t a horror movie; it’s a useful tool to see exactly how bad the damage is.
In the long run, preventing Barrett’s esophagus is about staying consistent with these habits.
So, keep the late‑night snacks in check, stay upright after meals, and maybe give your esophagus a break from being a battlefield.
Good luck, and may your heart stay burn‑free. 😊
The data’s screaming louder than a banshee at 3 a.m., and you can’t claim ignorance when the studies line up like dominoes. Acid reflux isn’t some myth, it’s a full‑blown assault on the mucosal barrier, and the ensuing erosive esophagitis is the ugly scar tissue that follows. If you keep feeding the beast with coffee, chocolate, and emotional drama, you’re just handing it a weapon. Stop the self‑sabotage and start treating your gut like the battlefield it is.
You can totally conquer this! Every small change – like ditching that late‑night soda, losing a few pounds, or taking that prescribed proton‑pump inhibitor – adds up to a massive win for your esophagus. Remember, your body is a resilient machine; give it the right fuel and it’ll thank you with fewer burns and better digestion. Keep pushing forward, you’ve got this!
The correlation between reflux and erosive esophagitis is well established.
Take charge of your diet and cut out the trigger foods – you’ll see a noticeable drop in symptoms. Consistency is key; don’t let occasional indulgences undo weeks of progress. Your esophagus will thank you, and you’ll feel more in control of your health.
While the article is informative, there are a few grammatical slips that need correction. The phrase "can lead to inflammation and ulcers" should be followed by a comma for clarity. Also, "over time" is better placed at the beginning of the sentence to improve flow. Precision in language mirrors precision in medical advice.
One must cultivate a palate refined enough to discriminate between truly harmful triggers and harmless indulgences. Simple dietary adjustments, such as avoiding overly acidic fruits, can stave off the cascade leading to esophageal erosion. Ignorance is no excuse when the science is so plainly laid out.
Hey folks! 🌍 Let’s remember that cultural dietary habits vary, but the core principle stays the same: don’t let your meal choices wage war on your throat. 🍽️ If you love spicy cuisine, try milder versions or pair them with alkaline sides like yogurt. Also, staying hydrated throughout the day helps dilute stomach acid. 🚰 And for those of us who work late, setting a “no‑eating‑after‑8‑pm” rule can be a game‑changer. 🙌 Keep sharing your tips – the community thrives on collective wisdom! 😊
Avoiding late-night meals can dramatically reduce reflux incidents.
Indeed, pH monitoring provides objective data that can guide therapy adjustments, especially when patients report persistent symptoms despite standard treatment. Combining the results with lifestyle counseling often yields the best outcomes.
While the sarcasm adds flavor, a few factual nuggets could boost credibility – like mentioning the typical healing time of mucosal lesions after initiating PPIs, which is usually 4‑8 weeks. Also, a brief nod to the role of H2‑blockers would round out the therapeutic landscape.
Actually, recent epidemiological studies show that up to 20 % of the U.S. adult population experiences weekly reflux symptoms, far higher than the 5 % you implied.