Doxycycline substitutes: what to use and when
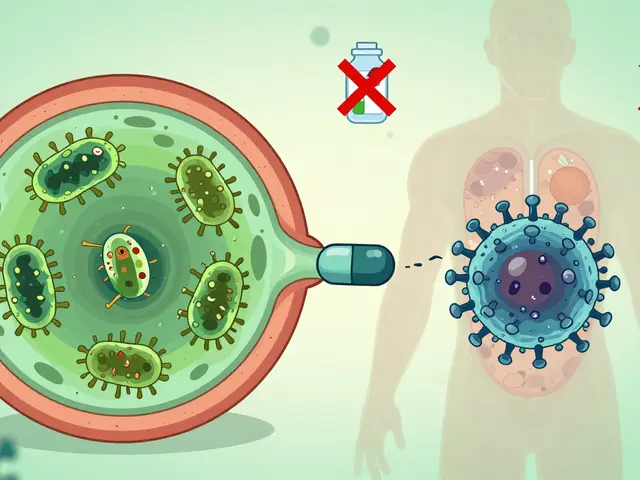
Need an alternative to doxycycline? Maybe you’re allergic, pregnant, nursing, treating a child, or worried about resistance. Whatever the reason, there are several solid options — but the right choice depends on the infection, age, pregnancy status, and local resistance patterns. Below I map common substitutes and the situations where each makes sense.
Common drug alternatives and when they fit
Azithromycin (a macrolide) — a go-to for many respiratory infections and some sexually transmitted infections. It’s often chosen when tetracyclines aren’t tolerated or can’t be used in pregnancy. It’s easy to take and usually well tolerated, but local resistance can limit its usefulness for certain chest infections.
Amoxicillin / ampicillin (penicillins) — excellent for many ear, throat, and sinus infections, and commonly used in children. Amoxicillin is a safe option in pregnancy and breastfeeding when doxycycline is off the table. It won’t work for infections caused by bacteria that make beta-lactamase unless paired with a beta-lactamase inhibitor.
Cephalosporins (cefuroxime, ceftriaxone) — useful for more serious or specific infections like Lyme disease or certain resistant respiratory bugs. Doctors often pick a cephalosporin when penicillin can’t be used, or when broader coverage is needed. Note: there’s a small cross-reaction risk if you have a severe penicillin allergy, so check with your provider.
Trimethoprim-sulfamethoxazole (TMP-SMX) — works well for many skin infections, including MRSA in some areas. It’s not suitable for everyone (pregnancy and some kidney conditions require caution), but it’s a reliable choice for community-acquired skin infections.
Clindamycin — a strong option for skin and soft-tissue infections and for some dental infections. It covers different bacteria than doxycycline, but it can cause stomach upset and increase the risk of C. difficile infection, so doctors weigh benefits and risks.
Fluoroquinolones (levofloxacin, moxifloxacin) — powerful for some lung and complicated infections. They’re used when other options fail or when oral step-down therapy is needed. Because of tendon and nerve risks and other side effects, clinicians avoid them for uncomplicated infections when safer options exist.
Picking the right substitute: quick tips
Ask these questions before accepting an alternative: Are you pregnant or breastfeeding? Are you under 8 years old? Do you have penicillin or sulfa allergies? Has the infection been cultured and tested for resistance? These answers narrow choices fast.
Other practical tips: always tell your clinician about recent antibiotic use and side effects; complete the full course even if you feel better; and alarm your provider if severe side effects appear (allergic reaction, high fever, severe diarrhea, or tendon pain with fluoroquinolones).
If you’re unsure which substitute is right, ask for culture-based testing or a clear explanation of risks and benefits. That short conversation can prevent treatment failure and avoid unnecessary side effects.
Want help matching a specific infection to alternatives? Tell me the type of infection, age, and pregnancy status and I’ll list the most likely substitutes and what to discuss with your prescriber.

Discover 5 Effective Alternatives to Vibramycin for Treating Infections
Explore five alternatives to Vibramycin, a commonly used antibiotic for treating infections. This article provides in-depth analysis of each substitute, discussing their advantages and disadvantages. Discover different options to meet diverse medical needs, ensuring effective treatment outcomes. The information aims to empower readers with choices and awareness in managing their health.
view more