
Medication Weight Change Estimator
How to Use This Tool
Select your medication class from the dropdown below to see estimated weight changes over 6 months. This calculator uses clinical data from the article to provide estimates.
How Weight Changes Work
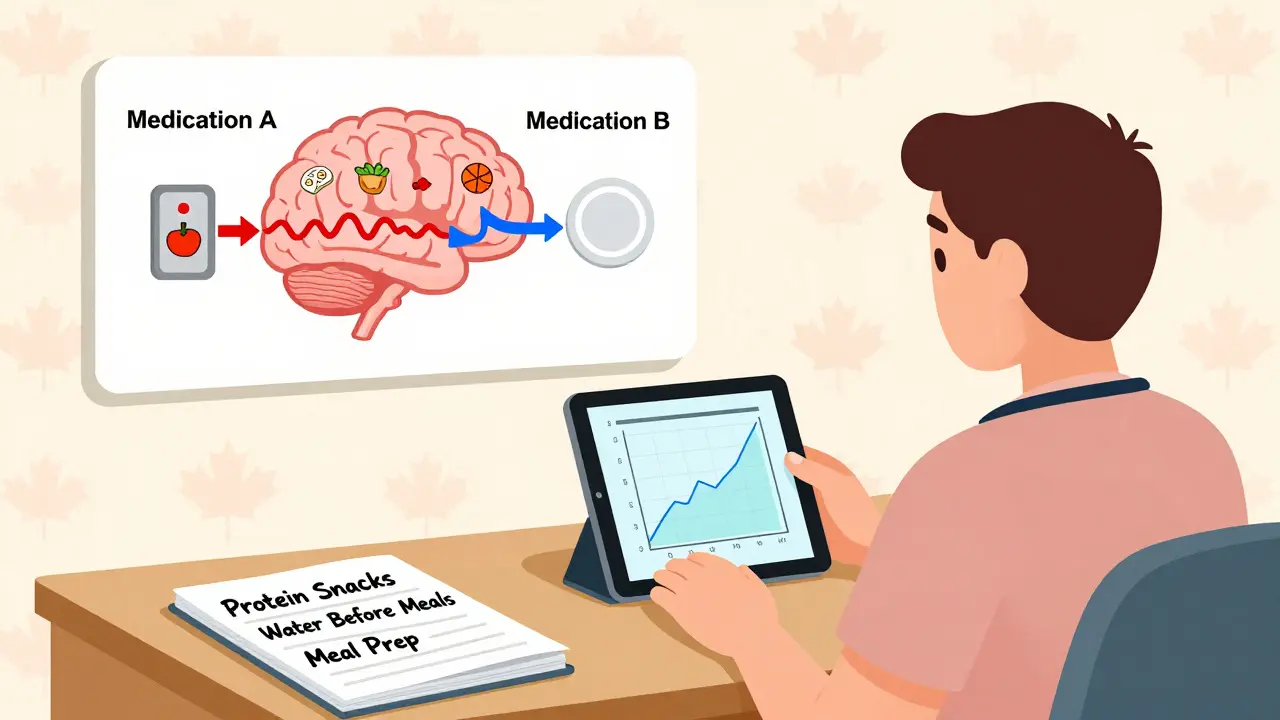
Medications affect your body's hunger and fullness signals through neurotransmitters like serotonin, dopamine, and histamine. Different medications have different effects on these signals, which can lead to weight gain or loss.
Important Note: This is an estimate based on clinical data. Individual results may vary based on factors like your metabolism, diet, exercise habits, and duration of use.
Many people don’t expect that a pill meant to help them feel better could make them hungrier-or less hungry-than before. But it’s more common than you think. Whether you’re taking antidepressants, antipsychotics, diabetes meds, or even allergy pills, your appetite can shift in ways that surprise, frustrate, or even worry you. Some gain weight without changing their eating habits. Others lose interest in food entirely, even when they know they need to eat. These aren’t just inconveniences-they can affect your health, confidence, and long-term treatment success.
Why Your Medication Changes Your Appetite
It’s not about willpower. It’s biology. Medications interact with your brain’s hunger and fullness signals, often through neurotransmitters like serotonin, dopamine, and histamine. These chemicals don’t just control mood-they tell your body when to eat, when to stop, and how to store energy. Take antipsychotics like olanzapine or quetiapine. They block histamine and serotonin receptors in the hypothalamus, the part of your brain that regulates hunger. Studies show this can raise ghrelin-the “hunger hormone”-by 15-20% within just four weeks. That’s why so many people on these drugs report constant hunger, even after eating. One user on Reddit described it as “a stomach that never feels full, no matter how much you eat.” Antidepressants work differently depending on how long you’ve been taking them. In the first few months, drugs like SSRIs may reduce appetite by boosting serotonin, which increases satiety. But after a year or more, your brain adapts. Serotonin receptors become less sensitive. That’s when cravings for carbs spike-up to 35% of long-term users report this shift. It’s not laziness. It’s your nervous system trying to balance itself. On the flip side, some meds suppress appetite. Amphetamines used for ADHD or narcolepsy increase norepinephrine and dopamine, which naturally reduce hunger. People on these drugs often skip meals without realizing it. Diabetes medications like insulin do the opposite-they help your body store glucose as fat, leading to weight gain of 2-4 kg in six months. Meanwhile, metformin helps you lose 2-3 kg in the same period. Same condition. Opposite effects.Which Medications Are Most Likely to Cause Appetite Changes?
Not all drugs affect appetite the same way. Some are notorious. Others are neutral-or even helpful. Here’s what the data shows:| Medication Class | Examples | Typical Appetite Effect | Average Weight Change (6 Months) |
|---|---|---|---|
| Second-gen antipsychotics | Olanzapine, quetiapine, risperidone | Strong increase | +4 to +10 kg |
| Antidepressants | Mirtazapine, amitriptyline, paroxetine | Increase | +2 to +5 kg |
| Antidepressants | Bupropion, vortioxetine | Neutral or decrease | -1 to +0.5 kg |
| Diabetes meds | Insulin, sulfonylureas | Increase | +2 to +4 kg |
| Diabetes meds | Metformin, GLP-1 agonists | Decrease | -2 to -5 kg |
| Mood stabilizers | Lithium | Moderate increase | +3 to +5 kg |
| Antihistamines | Diphenhydramine, hydroxyzine | Mild increase | +1 to +2 kg |
| Appetite suppressants | Topiramate, phentermine | Strong decrease | -3 to -5 kg |
Notice how mirtazapine stands out? It’s one of the most likely antidepressants to cause weight gain-up to 40% of users gain over 7% of their body weight in six months. Meanwhile, bupropion is one of the few that may help you lose weight. And topiramate, originally an anti-seizure drug, is now used off-label to counteract weight gain from other meds.
How to Manage Increased Appetite
If your medication is making you ravenous, you’re not powerless. Here’s what actually works, backed by clinical studies and user reports:- Plan protein-rich snacks every 3-4 hours. A snack with 15-20 grams of protein (like Greek yogurt, hard-boiled eggs, or cottage cheese) keeps blood sugar steady and reduces hunger spikes by 40%.
- Switch to whole grains. Replacing white bread, pasta, and rice with oats, quinoa, or brown rice increases satiety by 45 minutes per meal, according to Kelty Mental Health guidelines.
- Drink a glass of water 20 minutes before meals. In a group of 200 users, this simple habit cut daily calorie intake by 13% on average.
- Remove high-calorie snacks from sight. Behavioral studies show that just keeping junk food out of the house reduces impulsive eating by 35%.
- Meal prep twice a week. People who planned meals ahead ate 200 fewer calories per day than those who ate spontaneously.
- Try mindful eating. Slowing down, chewing thoroughly, and putting your fork down between bites reduces portion sizes by 15-20% without making you feel deprived.
One user on MyMoodMonitor switched from mirtazapine to bupropion and lost 15 pounds in six months-without worsening her depression. That’s not luck. It’s a smart swap, guided by a doctor.

How to Handle Loss of Appetite
If your meds are making food unappealing, your body still needs fuel. Skipping meals can lead to low energy, dizziness, or worse.- Eat small, frequent meals. Three small meals and two snacks a day are easier to manage than three big ones.
- Focus on calorie-dense, nutrient-rich foods. Add nut butter to toast, cheese to eggs, or olive oil to soups. You don’t need to eat more volume-you need more energy per bite.
- Use flavor to your advantage. If things taste bland, try herbs, lemon, garlic, or a splash of vinegar. Appetite often drops when food feels boring.
- Try liquid calories if solid food is hard. Smoothies with protein powder, full-fat yogurt, banana, and peanut butter can be easier to consume than a full meal.
- Move your body. Even a 15-minute walk before meals can stimulate appetite by increasing blood flow to the digestive system.
When to Talk to Your Doctor
Don’t wait until you’ve gained 10 pounds or lost 15% of your body weight. Early action makes all the difference.The Endocrine Society recommends checking your BMI and waist size at the start of treatment-and every three months after. Why? Because 80% of significant weight changes happen in the first six months.
Here’s when to speak up:
- Your weight changes by more than 5% in 3 months.
- You’re constantly hungry or feel full all the time.
- Your mood or energy is dropping because you’re not eating enough.
- You’ve tried lifestyle changes and nothing’s working.
Your doctor might suggest switching to a weight-neutral alternative. Vortioxetine, for example, causes only 0.5 kg of weight gain over six months-compared to 2.5 kg for older SSRIs. Or they might add metformin to help counteract insulin-related weight gain. In some cases, topiramate is prescribed specifically to reduce appetite from other meds.
But never stop or change your medication on your own. Abruptly quitting antipsychotics or antidepressants can trigger withdrawal, rebound depression, or even seizures. Tapering takes weeks-and it needs supervision.
The Bigger Picture: Why This Matters
Medication-induced appetite changes aren’t just personal-they’re a public health issue. In the U.S., 42.4% of adults have obesity. Experts estimate that 15-20% of those cases are linked to prescription drugs. That’s millions of people whose weight gain isn’t from overeating-it’s from their treatment.Healthcare is starting to catch up. The FDA now requires drug makers to report detailed weight change data for new psychiatric medications. Primary care doctors are screening for this side effect more often-65% now check weight during follow-ups, up from 35% in 2015.
And new drugs are coming. KarXT, a new antipsychotic in trials, caused only 0.4 kg of weight gain at five weeks-compared to 3.2 kg for olanzapine. That’s a game-changer.
Meanwhile, digital tools like Noom are helping people manage these changes with personalized coaching. One study showed 45% satisfaction with digital support-compared to 28% with standard advice.
What You Can Do Today
You don’t need to wait for a perfect solution. Start with these steps:- Track your weight weekly. Use a scale and note the date. Even small changes matter.
- Write down your hunger patterns. Are you hungrier after taking your pill? Does it fade by afternoon?
- Try one food change this week. Swap white rice for brown. Add a protein snack. Drink water before meals.
- Book a 10-minute chat with your doctor. Say: “I’ve noticed my appetite has changed since starting [medication]. Can we talk about whether this is normal or if we should adjust?”
Medications save lives. But they shouldn’t cost you your health. Managing appetite changes isn’t about willpower-it’s about understanding your body’s signals and working with your care team to find balance.
Can medication make you lose weight even if you’re not trying?
Yes. Some medications like amphetamines, topiramate, metformin, and GLP-1 agonists can reduce appetite and lead to weight loss-even without dieting. This is often intentional in diabetes or obesity treatment, but can be unexpected with antidepressants or ADHD meds. If you’re losing weight unintentionally and feel weak or dizzy, talk to your doctor.
Why do I crave carbs when I’m on antidepressants?
Long-term use of SSRIs and SNRIs can lower serotonin levels in your brain over time. Carbs temporarily boost serotonin, so your body craves them as a natural mood fix. This is why people on these meds often reach for bread, pasta, or sweets. Switching to whole grains and adding protein helps reduce these cravings without cutting out carbs entirely.
Is weight gain from medication permanent?
Not always. Many people lose weight after switching medications or adding metformin or topiramate. Behavioral changes like meal planning and protein snacks also help reverse gains. But the longer the weight stays on, the harder it is to lose. That’s why early intervention is key.
Can I take weight loss pills with my current medication?
Not without medical supervision. Many weight loss drugs interact with antidepressants, blood pressure meds, or diabetes treatments. For example, combining phentermine with an SSRI can increase the risk of serotonin syndrome. Always talk to your doctor before adding any new supplement or drug-even over-the-counter ones.
What if my doctor says the weight gain is normal and I should just accept it?
You have the right to ask for alternatives. If your medication is causing significant weight gain and affecting your health or mental well-being, ask: “Are there other options with less weight gain?” or “Can we try metformin or topiramate alongside this?” Many doctors now know about weight-neutral alternatives. If they don’t, ask for a referral to a specialist in psychopharmacology or metabolic health.






10 Comments
Okay but let’s be real - if your doctor prescribes olanzapine and doesn’t warn you about the ‘I ate an entire pizza at 2am and felt nothing’ effect, they’re doing you dirty. I gained 22 pounds in 4 months on this stuff and they acted like it was my fault for ‘not exercising enough.’ Bro, my brain thinks I’m starving even when I’m full. This isn’t laziness. It’s neurochemistry.
SSRIs increase satiety via 5-HT2C agonism. Long-term downregulation leads to carb cravings. Basic pharmacology.
Y’all are not alone. I was on mirtazapine for 18 months and went from 135 to 180 lbs without changing my routine. Then I switched to bupropion and started meal prepping protein bowls on Sundays. Lost 20 lbs in 5 months and my mood didn’t tank. You don’t have to suffer. Talk to your doc about alternatives - there are SO many now. And yes, drinking water before meals? Works. I swear by it. Also, keep snacks like almonds and hard-boiled eggs in your bag. Hunger hits fast - be ready.
The metabolic dysregulation induced by H1 and 5-HT2A antagonism in second-generation antipsychotics is a well-documented phenomenon. Ghrelin upregulation, insulin resistance, and leptin suppression are core mechanisms. You’re not ‘hungry’ - your hypothalamic-pituitary-adrenal axis is pharmacologically hijacked. The solution isn’t ‘snacks’ - it’s pharmacovigilance and metabolic monitoring protocols. If your clinician isn’t tracking HbA1c and waist circumference quarterly, they’re negligent.
People just need to stop being lazy. If you’re eating too much, just stop. No one’s forcing you to eat pizza at 3am. It’s called willpower.
Actually, the serotonin receptor downregulation theory is outdated. Recent fMRI studies show that chronic SSRI use alters orbitofrontal cortex valuation signals - it’s not about serotonin depletion, it’s about reward system reweighting. Carbs become hyper-palatable because the brain assigns them higher incentive salience. That’s why willpower fails. It’s not a moral failing - it’s neuroplasticity.
i just wanted to say thank you for this post. i’ve been on lithium for 5 years and i’ve gained like 30 lbs and i felt so guilty. but now i realize it’s not me. it’s the med. and i’m gonna talk to my dr about metformin. thank you thank you thank you
Did you know Big Pharma knows exactly how to make you gain weight so you’ll need more meds to fix the problems the first meds caused? They’re not trying to heal you - they’re trying to keep you dependent. Look at the numbers - 80% of weight gain happens in the first six months. Coincidence? Or design? I’m not taking anything anymore. I’m going herbal. Chamomile tea and turmeric. No more pills. No more corporations controlling my body
I was on topiramate for seizures and lost 18 lbs without trying. Then I got depression and started on sertraline - gained it all back and then some. Now I’m stuck in this loop. My doctor says ‘just eat less’ but I can’t even smell food without feeling nauseous. This system is broken.
Interesting how the article mentions KarXT but doesn’t mention that it’s still in Phase 3 trials. Don’t get your hopes up. Also, Noom? That’s a cult. Their ‘coaches’ are unpaid gig workers with no medical training. You’re better off just reading peer-reviewed journals.