
Every year, thousands of people in the U.S. and UK end up in emergency rooms because someone didn’t recognize the signs of a sedative or sleep medication overdose until it was too late. These aren’t just pills you take before bed-they’re powerful drugs that slow down your brain and body. When too much builds up, your breathing can stop. And if no one notices in time, it’s often fatal.
What Counts as an Overdose?
An overdose doesn’t always mean swallowing a whole bottle. Sometimes, it’s just one extra pill mixed with alcohol-or taking a prescription meant for someone else. Even people who’ve been using their medication for years can slip into overdose if they increase the dose, mix it with other depressants, or develop tolerance without realizing it.The most common culprits are benzodiazepines like alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin), along with the so-called "Z-drugs" like zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata). Barbiturates are less common now but still dangerous. Even over-the-counter sleep aids like diphenhydramine (Benadryl, Tylenol PM) can cause serious harm at high doses.
Here’s the truth: these drugs are not harmless. In 2021, over 12,500 deaths in the U.S. involved benzodiazepines alone. Many of those deaths happened because someone didn’t know what to look for.
The Early Warning Signs
The first signs are easy to miss. They look like deep sleep, exhaustion, or even just being "out of it." But there’s a difference between being sleepy and being in danger.- Unresponsive to loud noise or physical stimulation-shaking them hard, yelling their name, rubbing their sternum-won’t wake them up. Normal sleepers will stir. Someone overdosing won’t.
- Slurred speech-like they’re drunk, but they haven’t had alcohol. This happens in nearly 9 out of 10 cases.
- Extreme confusion-they can’t answer simple questions like "Where are you?" or "What day is it?"
- Loss of coordination-stumbling, dropping things, inability to stand without help. This is called ataxia.
These symptoms don’t appear suddenly. They creep in. A person might seem a little dazed after dinner, then more sluggish by bedtime, then completely out of it by morning. That’s not normal fatigue. That’s a warning.
The Life-Threatening Signs
If the early signs are ignored, the body starts shutting down. This is when minutes matter.- Shallow or slow breathing-count their breaths for 30 seconds. If they take fewer than 6 breaths in that time (less than 12 per minute), they’re in critical danger. Normal is 12-20.
- Blue lips or fingertips-this is cyanosis. It means their blood isn’t getting enough oxygen. Their skin may also feel cold and clammy.
- Heart rate below 50-though some sedatives don’t crash the heart right away, the combination of slow breathing and low oxygen will eventually cause it to slow dangerously.
- Coma-if they’re completely unresponsive and their Glasgow Coma Scale score is below 8, they’re in a drug-induced coma. Survival drops sharply after this point.
Respiratory failure is the #1 cause of death in sedative overdoses. The CDC says it accounts for 92% of fatal cases. And here’s the scary part: people often don’t realize breathing has stopped until it’s too late. Their chest isn’t rising. No sound. No movement. Just silence.
What Makes It Worse?
Not all overdoses are the same. Some combinations are deadly.Alcohol is the most common dangerous mix. Nearly 4 in 10 fatal sedative overdoses involve alcohol. Together, they double down on brain suppression. The same goes for opioids. In 2021, 23% of benzodiazepine-related deaths also involved fentanyl. That combination is a silent killer-it slows breathing so much, people often don’t even gasp before they stop.
Over-the-counter sleep aids like diphenhydramine behave differently. At high doses, they can cause hallucinations, seizures, or urinary retention-not just sleepiness. Melatonin, on the other hand, is rarely dangerous-even at 60 times the normal dose, it causes headaches and nausea, not respiratory failure.
Barbiturates are the most lethal class. They depress breathing at lower doses than benzodiazepines. That’s why they’re rarely prescribed today-but if someone is still taking them, the risk is much higher.
What to Do If You Suspect an Overdose
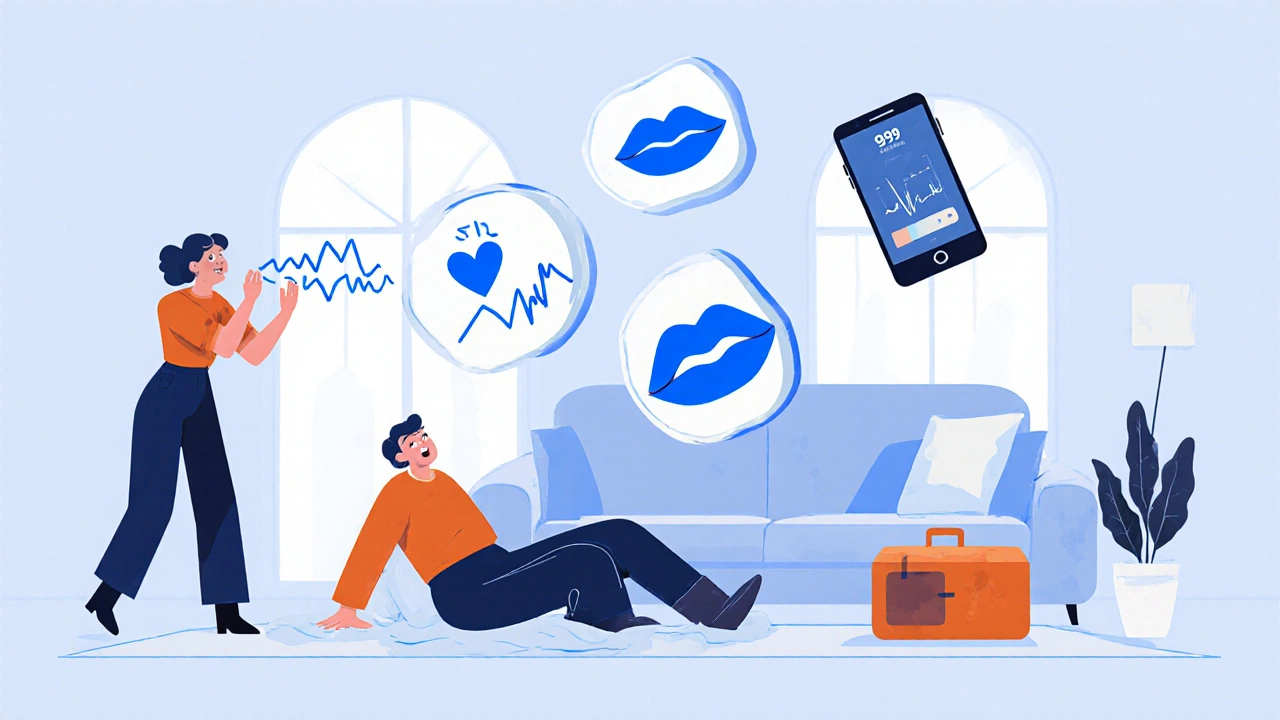
Time is everything. Every minute you wait reduces the chance of survival by 7-10%.Step 1: Check responsiveness. Shout their name. Shake their shoulder hard. Try a sternal rub-rub your knuckles firmly against the center of their chest. If they don’t react at all, assume it’s an overdose.
Step 2: Check breathing. Look at their chest. Count how many times it rises in 30 seconds. Multiply by two. If it’s less than 12 per minute, call 999 immediately.
Step 3: Look for blue lips or cold skin. These are late signs-but they mean the body is failing. Don’t wait for them.
Step 4: Call emergency services. Don’t hesitate. Don’t wait to see if they "wake up on their own." Say: "I think someone overdosed on sleep meds." Give your location. Stay on the line.
Step 5: If they’re not breathing, start rescue breathing. Tilt their head back, lift the chin, pinch the nose, and give one breath every 5 seconds. Don’t stop until help arrives or they start breathing on their own.
Do NOT give them coffee, cold showers, or try to make them walk. These myths can kill. Do NOT give them flumazenil (the reversal drug). It can trigger seizures in people who’ve been using sedatives regularly.
What You Might See in Real Life
People don’t always recognize the signs. A 2022 study found that 68% of bystanders thought someone was just "really tired" or "drunk." One Reddit user wrote: "I thought my roommate was just exhausted from work. He didn’t move all night. I didn’t call 999 until the next morning. He was lucky to survive." Another said: "I assumed the slurred speech was from drinking. He didn’t even have a glass in his hand." These aren’t rare stories. The National Poison Data System logged over 46,000 sedative exposures in 2022. Most happened at home. Most were missed until it was almost too late.
How to Prevent It
- Never mix sedatives with alcohol or opioids. Ever. - Keep medications locked up, especially if others live in the house. - Don’t take someone else’s prescription-even if they say it’s "just for sleep." - If you’ve been on these meds for months, talk to your doctor about tapering. Tolerance builds fast. - If you or someone you know is using these to cope with anxiety or trauma, get help. These drugs mask problems, they don’t fix them. - Keep a list of all medications someone is taking. Many overdoses happen because doctors don’t know what else the patient is using.Pharmacies in places like California now hand out free overdose recognition cards. They show the key signs in simple pictures. You can ask your pharmacist for one-even if you’re not the one taking the meds.
What’s Changing Now
New tools are emerging. Pulse oximeters that clip onto a finger can now warn you if oxygen levels drop before breathing stops. Johns Hopkins researchers are testing these in homes for high-risk patients. Early results show they can give 15-20 minutes of warning.Emergency rooms are now screening patients for sedative misuse using a simple 8-question test. It catches 94% of people at risk.
The FDA added stronger warnings to sleep medications in April 2023. They now say: "These drugs can cause serious injury or death if misused." That’s not a footnote. That’s a headline.
You don’t need to be a doctor to save a life. You just need to know what to look for-and act fast.
Can you overdose on sleep meds even if you take them as prescribed?
Yes. People can accidentally overdose even when following their prescription if they mix the medication with alcohol, become tolerant over time, or take it with other drugs that depress the nervous system. Some people metabolize these drugs slower than others, which can lead to buildup. Always check with your doctor before combining medications.
How long does it take for sedatives to cause an overdose?
It depends on the drug, the dose, and whether it’s mixed with other substances. Some pills take 30-60 minutes to peak. Alcohol can speed up absorption. In combination cases, respiratory depression can happen in under 20 minutes. There’s no safe waiting period-if someone becomes unresponsive, act immediately.
Is it safe to let someone "sleep it off" after taking too many sleep meds?
No. This is one of the most dangerous myths. Sedative overdose doesn’t resolve on its own. Breathing can stop without warning. Even if they’re breathing now, their condition can worsen rapidly. Every minute counts. Call emergency services immediately if they’re unresponsive or breathing less than 12 times per minute.
Can flumazenil be used at home to reverse a sedative overdose?
No. Flumazenil is a hospital-only drug. Giving it outside a medical setting can trigger seizures, especially in people who’ve been using benzodiazepines regularly. The FDA has documented fatal seizures from improper use. Never attempt to use it without professional supervision.
Are newer sleep meds like Ambien safer than older ones?
They were marketed as safer, but studies show they carry similar overdose risks. The death rate from zolpidem (Ambien) has risen sharply since the 1990s. While they may be less toxic in isolated cases, mixing them with alcohol or opioids makes them just as deadly as older drugs. Safety depends on use, not the brand name.
What should I do if I find an empty pill bottle next to an unresponsive person?
Call 999 immediately. Don’t wait. Don’t try to figure out what it was. Take the bottle with you to the hospital-it helps medics choose the right treatment. Even if you’re unsure, better to overreact than underreact. Your action could save a life.






10 Comments
These signs are so quiet. Like watching a candle flicker out.
People think if it's prescribed it's safe
But your brain doesn't care if the pill came from a doctor or a stranger
It just knows the chemistry
And when the chemistry turns against you
You don't get a second chance
Stop treating sedatives like tea
Turned out it was his sleeping pills
He woke up 3 hours later
Didn't say a word
We never talked about it again
To anyone reading this: if you’re scared to call because you think you’re overreacting-you’re not. You’re the hero in this story. Don’t wait for permission to save someone. Just act.
❤️