Renal Dosing Calculator
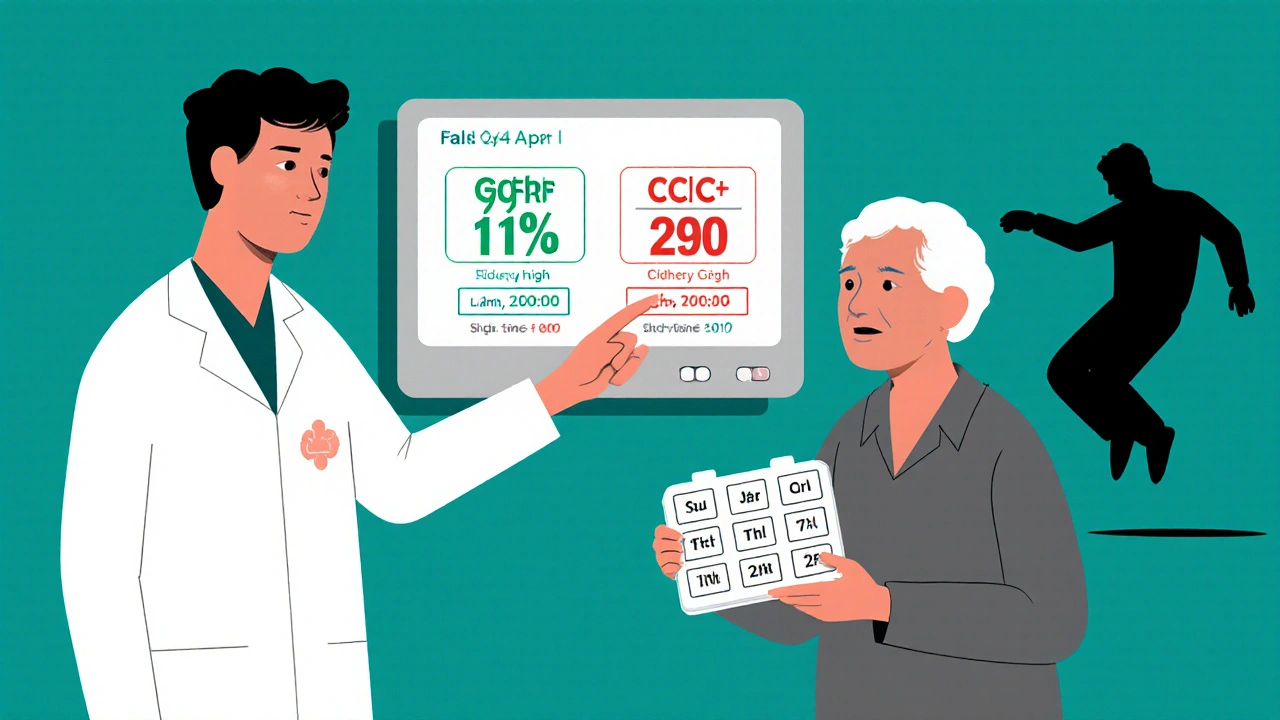
This calculator uses the Cockcroft-Gault formula, recommended by guidelines for dosing decisions in older adults. Note: CrCl estimates kidney function but should be interpreted by a healthcare professional.
When you're over 65 and your kidneys aren't working like they used to, even a normal dose of a common medication can turn dangerous. It's not about taking too much-it's about your body not clearing it the way it used to. About 38% of adults 65 and older have some level of chronic kidney disease. That means nearly four in ten older adults are at risk for drug toxicity simply because their kidneys can't keep up. And it’s not rare. It’s happening every day in homes, nursing facilities, and hospitals-often unnoticed until it’s too late.
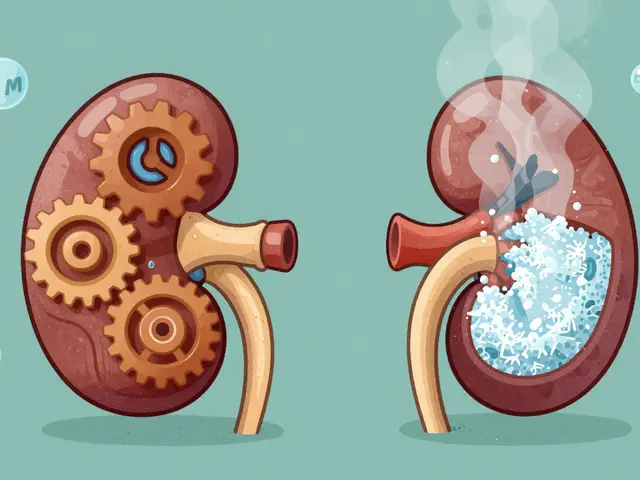
Why Kidneys Matter More as You Age
Your kidneys don’t just filter waste. They control how long drugs stay in your body. As you get older, kidney function naturally declines. Glomerular filtration rate (GFR), the measure of how well your kidneys filter blood, drops by about 1% per year after age 40. By 70, many people have less than half the kidney function they had in their 20s. But here’s the problem: doctors still often prescribe the same doses they’d give to a 40-year-old. That’s where things go wrong. Medications like gabapentin, digoxin, metformin, and certain antibiotics are cleared mostly by the kidneys. When kidney function drops, these drugs build up. The result? Confusion, dizziness, falls, irregular heartbeats, even coma. In fact, studies show that 12-15% of all serious drug reactions in older adults happen because kidney dosing wasn’t adjusted.How Do You Know If Your Kidneys Are Impaired?
You can’t feel your kidneys slowing down. There’s no pain, no warning sign. The only way to know is through a simple blood test: serum creatinine. From that, doctors calculate your estimated kidney function using one of two equations: Cockcroft-Gault or MDRD. The Cockcroft-Gault equation is the most commonly used for dosing. It uses your age, weight, sex, and creatinine level. The formula looks like this:CrCl = [(140 - age) × weight (kg)] ÷ (72 × serum creatinine) × 0.85 (if female)
But here’s the catch: this formula can underestimate kidney function in elderly people by 15-20%. Why? Because older adults often have less muscle mass. Creatinine comes from muscle. Less muscle = lower creatinine = falsely high estimated kidney function. So even if your creatinine looks normal, your kidneys might be weaker than the number suggests.
That’s why guidelines now recommend using the Cockcroft-Gault equation for dosing decisions in older adults-not the MDRD or eGFR numbers you see on lab reports. MDRD is better for research. Cockcroft-Gault is better for safety.
Which Medications Are Most Dangerous?
Not all drugs are equal when it comes to kidney risk. Some are safe. Others are ticking time bombs. Here are the big ones:- Metformin - Used for diabetes. In the U.S., it’s banned if creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But in Europe, it’s still used with close monitoring. The risk? Lactic acidosis-a rare but deadly buildup of acid in the blood.
- Gabapentin - For nerve pain and seizures. Up to 68% of prescribers get the dose wrong in elderly patients. Normal dose? 300-1200 mg daily. With CrCl under 30 mL/min? Cut it to 300 mg once a day. Too much? Drowsiness, falls, confusion.
- Digoxin - For heart failure. Therapeutic range is tiny: 0.8-2.0 ng/mL. Too high? Nausea, blurry vision, irregular heartbeat. In elderly patients with low kidney function, levels can spike even on low doses. Always check levels 15-20 days after starting or changing dose.
- Lithium - For bipolar disorder. Safe level? 0.6-0.8 mmol/L. Kidneys clear it. If kidney function drops, lithium builds up fast. Many older patients end up hospitalized because no one checked their levels.
- Allopurinol - For gout. Standard dose? 100 mg daily. But if CrCl is below 10 mL/min? Start with 100 mg every other day. Too much? Life-threatening skin reactions.
- Cefepime - An antibiotic. Standard dose? 1 gram every 6 hours. With CrCl 10-29 mL/min? Change to 1 gram every 12 hours. Below 10 mL/min? 1 gram every 24 hours. Miss the adjustment? Seizures.
Some drugs, like glipizide (another diabetes pill), don’t need dose changes even with poor kidney function. But you won’t know unless you check the guidelines. That’s why a one-size-fits-all approach fails.
The 50% Rule-And Why It’s Not Enough
Many doctors use a shortcut: if a drug is more than 50% cleared by the kidneys, cut the dose in half when CrCl drops below 50 mL/min. It’s simple. But it’s also wrong for many drugs. Take vancomycin. It’s cleared by the kidneys, but its clearance isn’t linear. Cutting the dose by 50% might still leave you with toxic levels. The right move? Extend the time between doses-from every 12 hours to every 48 hours. That’s interval extension, not dose reduction. Or take piperacillin/tazobactam. The right adjustment? Reduce the dose AND lengthen the interval. That’s a combo approach. The 50% rule doesn’t cover that. And that’s why 22% of high-risk medications don’t respond to simple rules.What Works in Real Life?
It’s not enough to know the guidelines. You have to use them. A 2015 study found that only 43.7% of prescribers consistently adjusted doses for elderly patients. The biggest mistakes? Gabapentin, rivaroxaban, and allopurinol. Why? Because no one checked the kidney numbers. Or they trusted the lab’s eGFR without knowing it was inaccurate. The solution? Systems. At the University of Nebraska Medical Center, they added alerts to their electronic health record. When a doctor prescribed cefepime to a patient with CrCl under 30, the system popped up: “Adjust dose to q12h.” Within a year, inappropriate dosing dropped by 37.2%. At the Mayo Clinic, clinical pharmacists took over dosing for patients over 65 on renally cleared drugs. Result? A 58% drop in adverse drug events. Even simple tools help. Apps like Epocrates Renal Dosing have been downloaded over 1.2 million times. They let you plug in age, weight, creatinine-and get instant dosing recommendations for 150+ drugs.What’s Changing Now?
The field is evolving. In 2023, the FDA approved the first AI-powered dosing tool: DoseOptima. It pulls data from your EHR, calculates your true kidney function using cystatin C (a better marker than creatinine for older adults), and recommends exact doses. In a trial of 15,000 patients, it was 92.4% accurate. KDIGO, the global kidney health group, is updating its guidelines to recommend cystatin C as the preferred test for elderly patients. Why? Because it’s not affected by muscle mass. It’s a more honest measure of kidney function. And the Beers Criteria-the list of risky medications for older adults-now includes 32 drugs with specific renal dosing rules. If you’re prescribing one of these, you’re expected to adjust.What You Can Do
If you or a loved one is over 65 and taking multiple medications:- Ask for a serum creatinine test if you haven’t had one in the last 6 months.
- Ask your doctor: “Is this drug cleared by the kidneys? What’s my CrCl?”
- Ask for a medication review-especially if you’ve been hospitalized or had a fall.
- Use a pill organizer with clear labels. Don’t rely on memory.
- Keep a list of all medications, including over-the-counter and supplements. Bring it to every appointment.
Don’t assume your doctor knows. Many don’t. A 2018 study found that 20-30% of dosing errors happen because doctors rely on estimated GFR without checking the context.
Why This Matters More Than You Think
This isn’t just about avoiding side effects. It’s about staying independent. A single toxic dose of gabapentin can lead to a fall. A fall can mean a hip fracture. A hip fracture can mean losing your independence. And for older adults, that’s often the beginning of the end. Hospitals are now financially penalized for drug-related harm. Medicare can take away 1% of a hospital’s payments-about $17,000 per bed-per year if they have too many adverse drug events. That’s why some hospitals now have pharmacists on rounds, checking every dose for every elderly patient. The cost of getting it right? A few minutes of time. The cost of getting it wrong? Your life.How do I know if my kidney function is low?
Your doctor can check your kidney function with a simple blood test for serum creatinine. From that, they calculate your creatinine clearance (CrCl) using the Cockcroft-Gault formula. If your CrCl is below 60 mL/min, your kidneys are impaired. But don’t rely on the eGFR number on your lab report-it’s often inaccurate for older adults. Ask for CrCl specifically.
Can I still take metformin if I have kidney problems?
In the U.S., metformin is typically stopped if serum creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But in Europe, it’s often continued with close monitoring if CrCl is above 30 mL/min. The risk is lactic acidosis, which is rare but serious. Always discuss your options with your doctor-don’t stop it on your own.
What’s the most common mistake doctors make with elderly kidney dosing?
The biggest mistake is using estimated GFR (eGFR) instead of Cockcroft-Gault CrCl for dosing decisions. eGFR can overestimate kidney function in older adults by 15-20% because it doesn’t account for low muscle mass. This leads to underdosing of some drugs and dangerous overdosing of others. Always ask for CrCl.
Are over-the-counter drugs safe for elderly kidneys?
No. NSAIDs like ibuprofen and naproxen can sharply reduce kidney blood flow and worsen kidney function. Even daily use of these painkillers can cause harm in older adults. Acetaminophen is safer, but still needs caution if liver function is also poor. Always check with your pharmacist before taking any OTC drug regularly.
Should I get my kidney function checked every year?
Yes-if you’re over 65 and taking any medications, especially for diabetes, heart disease, or chronic pain. Kidney function changes slowly, but it changes. A yearly blood test is one of the simplest ways to prevent a serious drug reaction. Ask for serum creatinine and CrCl calculation.




13 Comments
man i just had my grandpa on gabapentin and he kept falling like a sack of potatoes. doc said 300mg 3x a day. turns out his crcl was 22. they finally cut it to 300mg once and he stopped turning into a zombie. why the hell do they still give normal doses to old folks? it's like they think we're all 30 and jacked
While the Cockcroft-Gault equation remains the gold standard for renal dosing in the elderly, it is critical to recognize that muscle mass decline is not the only confounding factor. Sarcopenia, frailty, and nutritional status all interact with creatinine production. Recent studies suggest that combining cystatin C with adjusted Cockcroft-Gault improves predictive accuracy by up to 27%. The FDA's DoseOptima tool, while promising, still requires manual verification in patients with complex comorbidities. Always cross-reference with clinical context, not just algorithms.
thank you for this. my mom is 72 and on 4 meds that i now know are risky. i printed out the list and took it to her dr. she cried because she felt like she'd been ignored for years. this isn't just science-it's dignity. 🙏
It is a matter of profound concern that renal dosing protocols in many healthcare systems remain outdated, particularly in resource-constrained environments where laboratory access is limited. The reliance on eGFR, which systematically overestimates renal function in elderly patients with low muscle mass, constitutes a systemic failure in geriatric pharmacovigilance. Institutional protocols must mandate the use of Cockcroft-Gault for dosing decisions in patients above 65, irrespective of the eGFR value displayed on laboratory reports.
we need to stop treating elderly patients like young people with wrinkles. my uncle got hospitalized because his doctor didn't adjust his allopurinol. he got a skin reaction so bad he lost 15 lbs. if we had checked his CrCl earlier, none of this would've happened. doctors need training-not just guidelines. teach them to ask: is this drug cleared by kidneys? what's the real CrCl? not the eGFR they see on the screen.
It is noteworthy that the 50% rule, while intuitively appealing, lacks pharmacokinetic rigor for many renally cleared agents. Vancomycin, for instance, exhibits non-linear clearance kinetics, necessitating interval extension rather than dose reduction. Similarly, piperacillin/tazobactam requires both dose and interval modification. The oversimplification of dosing algorithms contributes significantly to adverse drug events in the elderly population.
Check creatinine. Ask for CrCl. Don't trust eGFR. Simple. Do this for your parents. Save their life.
we're all just meat machines with broken filters and someone else's math on the dashboard. the body doesn't care about your lab report. it cares about what's actually in the blood. the system is built on assumptions that died with the 1980s. we're measuring youth in old bones and calling it science. but what is science if not just a story we tell ourselves until the truth comes crashing in?
my grandma died after a fall from gabapentin. they said it was 'just aging'... but it wasn't. it was a dose that should've been cut in half. now i carry her meds list in my phone. every time i see a dr i say 'crcl please'. no more guesses. no more 'oh we'll monitor'. i'm tired of waiting for the next tragedy. if you're over 65 and on meds-ask for crcl. it's not optional. it's survival
india has better kidney care than usa. we know old people have less muscle. we check creatinine before giving any medicine. you americans just throw pills at people and hope they dont die. your system is broken. your doctors are lazy. your hospitals care about money not lives
you think crcl is the answer? lol. i had my creatinine at 1.2 and my crcl was 58 but i was super weak and had no muscle. turns out my real kidney function was like 35. the formula is garbage. we need better tests. like the new cystatin c thing. why are we still using 1970s math on 2020s bodies?
let me be brutally honest-this isn't about kidney function. it's about the quiet, invisible genocide of the elderly. we treat them like obsolete machines, not human beings who spent decades building this world. we give them doses meant for 30-year-olds because it's easier, cheaper, faster. we don't want to think about their fragility. we don't want to sit with them while their bodies fail. so we medicate them into silence, into falls, into hospitals, into death-and call it 'standard care'. this post? it's not medical advice. it's a funeral notice written in pharmacology. and we're all complicit.
bro i just checked my mom's last lab-eGFR said 65 so doc didn't touch her metformin. i pulled up cockcroft-gault and her crcl was 38. i showed the doc and he changed it. turns out he never even looked at the formula. just trusted the eGFR. this is wild. we need to start teaching this in med school