When you’re managing bipolar disorder with lithium carbonate, the brand on the bottle isn’t just a label-it can change your blood levels, your side effects, and even your risk of hospitalization. This isn’t theoretical. Real patients have ended up with lithium levels above 1.8 mmol/L after switching from one generic to another, leading to tremors, confusion, and emergency room visits. Why? Because lithium carbonate is an NTI drug-a narrow therapeutic index medication. That means the difference between a therapeutic dose and a toxic one is razor-thin. And with generics, that line can shift without warning.
Why Lithium Isn’t Like Other Medications
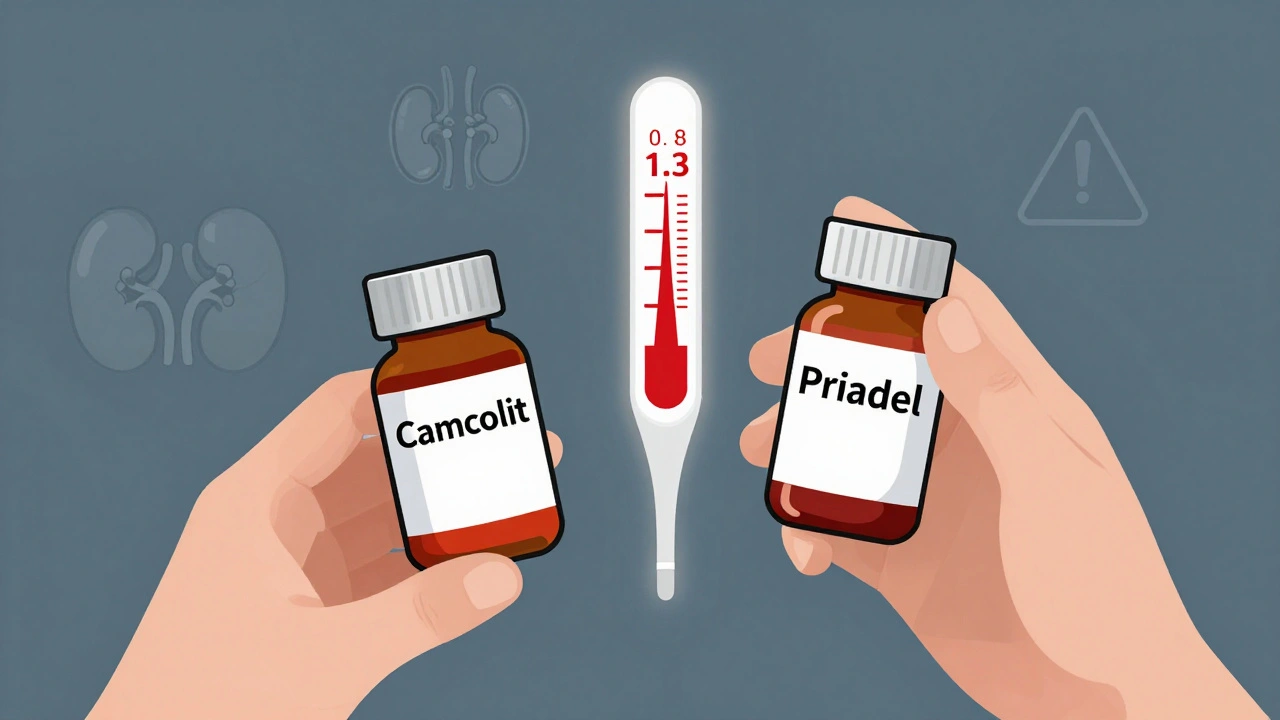
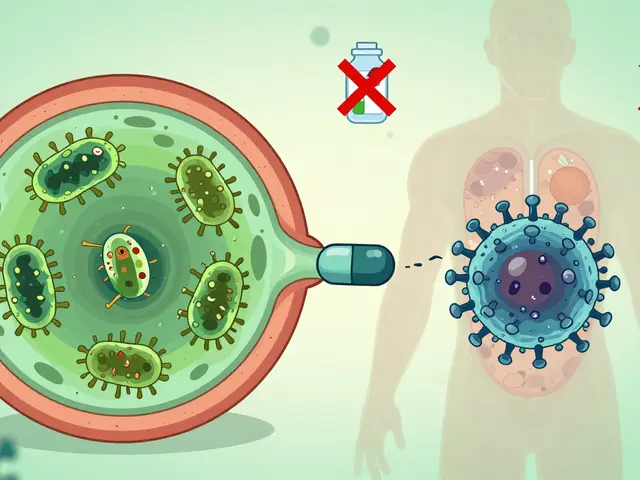
Most drugs have a wide safety margin. Take ibuprofen: you can take 400 mg or 800 mg and still be fine. Lithium? The therapeutic range is 0.6 to 1.2 mmol/L. Go above 1.5 mmol/L, and you’re in danger. Above 2.0 mmol/L, and you risk seizures, kidney failure, or cardiac arrest. That’s why every patient on lithium needs regular blood tests. But here’s the catch: two different generic versions of lithium carbonate, both labeled as 300 mg, can produce different blood levels in the same person. This isn’t because one is “better” or “worse.” It’s because of how they’re made. Immediate-release generics dissolve quickly in the stomach, spiking blood levels within 1-2 hours. Sustained-release versions, like Priadel or Camcolit, release lithium slowly over 4-5 hours. That changes everything-how often you need to test, what your target level should be, and how your body handles the drug.The Real Difference Between Generics
A 2024 study in the Journal of Psychopharmacology tracked over 200 patients switching between generic lithium formulations. When patients moved from Camcolit to Priadel, their average serum levels jumped by 11%. That’s not a fluke. It happened consistently. And yet, when researchers adjusted for age, weight, and kidney function, the brand difference disappeared. What does that mean? It means the problem isn’t the generic itself-it’s the switch. Think of it like this: two cars with the same engine size can have different fuel efficiency based on tire pressure, transmission tuning, or aerodynamics. Lithium generics work the same way. Even if they’re both “bioequivalent” under FDA rules (80-125% of the brand’s absorption), that’s a huge range. One generic might release lithium at 85% of the brand’s rate. Another at 115%. For a drug with a 0.6-1.2 mmol/L window, that’s enough to push someone from safe to toxic.What Your Target Level Should Be
There’s no single “right” level. It depends on what you’re treating and how you’re taking it.- For acute mania: 0.8-1.0 mmol/L is standard. Studies show this range cuts relapse risk by more than half compared to lower levels.
- For long-term maintenance: 0.6-0.8 mmol/L is now widely recommended, especially for older adults or those with kidney issues.
- For sustained-release formulations: Aim for the higher end of the range-0.8-1.0 mmol/L. Because the drug releases slowly, your peak level is lower, so you need to maintain a higher average.
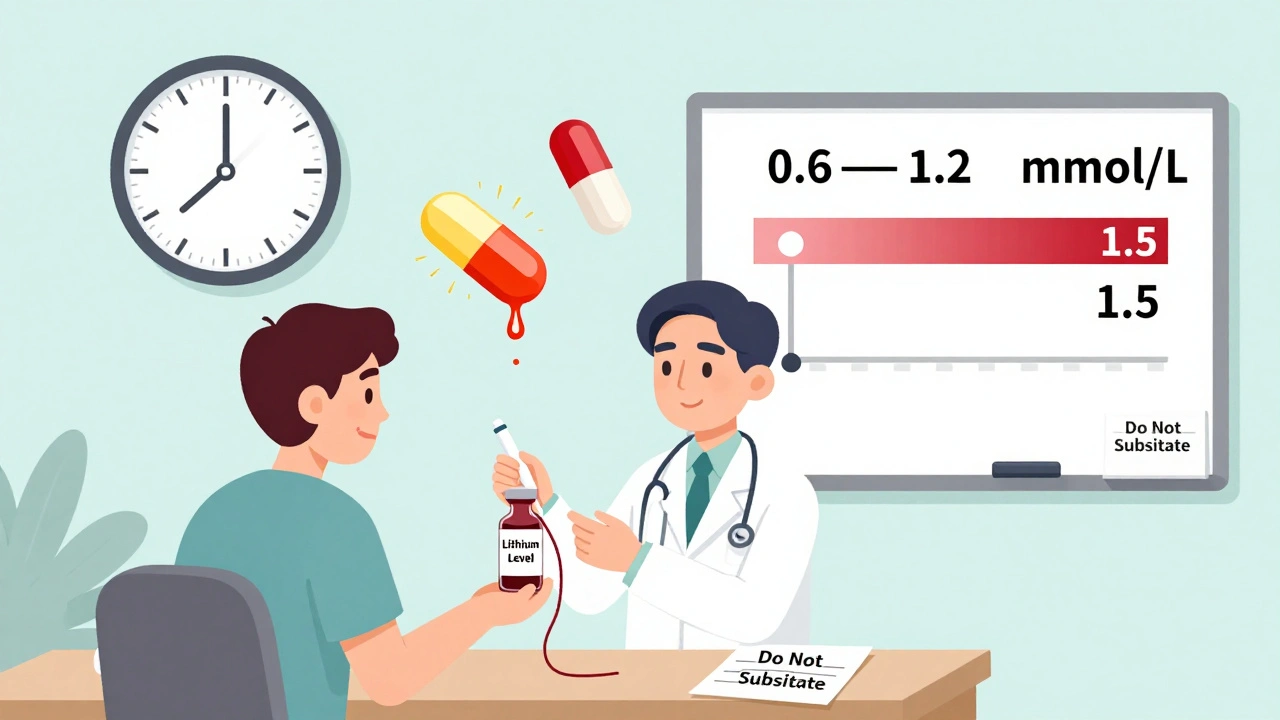
When to Test Your Levels
Timing matters. If you take lithium twice a day, your blood should be drawn 12 hours after your last dose. That’s when levels stabilize. If you take a once-daily sustained-release tablet, test 24 hours after your last dose. Get it wrong, and you’ll see a falsely low or high number. Testing frequency depends on your stability:- Starting lithium: Test weekly until levels stabilize.
- Dose changes: Test 5-7 days after any adjustment.
- Stable on maintenance: Every 3-6 months.
- After switching generics: Test within 1 week. Seriously. Don’t wait.
Who’s at Higher Risk?
Not everyone handles lithium the same way.- People over 60: Kidney function drops naturally with age. Many experts recommend reducing target levels by 20-25%. A 70-year-old might do fine at 0.5-0.7 mmol/L.
- Women: On average, women need lower doses than men-about 96 mg less per day-due to differences in body weight and water retention.
- People with kidney disease: Avoid lithium if your eGFR is below 30 mL/min. Even mild impairment requires tighter monitoring.
- Those on diuretics or NSAIDs: These drugs reduce lithium clearance. A common cold pill like ibuprofen can push your level up by 30-50%. Always check with your doctor before taking anything new.
What Happens When You Switch Brands
This is the silent danger. Pharmacists often substitute generics automatically. You might get Priadel one month, then Camcolit the next, then a no-name generic from a different manufacturer. Each one has a slightly different release profile. And your body doesn’t know the difference-it just reacts to the change in blood levels. In the same 2024 study, four patients developed toxic levels (1.32-1.88 mmol/L) after an unplanned switch. One needed hospitalization. None of them had their levels checked after the switch. If you’re on lithium, you need to know:- What brand you’re on
- Whether it’s immediate or extended-release
- That you must ask your pharmacist to not substitute without telling you
- That you must get a blood test within a week of any switch
What’s Changing in 2025
The FDA is finally catching up. In 2023, they released draft guidance requiring manufacturers of extended-release lithium to prove equivalence through actual human studies-not just lab tests. That’s a big deal. It means future generics will have to show they behave the same way in your body, not just in a test tube. Researchers are also exploring genetic markers. The International Consortium on Lithium Genetics has identified 30 genes that influence how your body processes lithium. In the next 5 years, we may see tests that tell you whether you’re a “high responder” or “low clearance” type-letting doctors personalize your dose before you even start. Meanwhile, some clinics are testing AI tools that pull data from your EHR-your age, weight, kidney function, meds, and past levels-to predict your ideal dose. It’s early, but it’s promising.Bottom Line: Don’t Assume Generics Are Interchangeable
Lithium carbonate generics are cheaper. That’s good. But they’re not all the same. If you’re on lithium, your blood level is your lifeline. Treat it like your glucose if you have diabetes. Check it regularly. Know your brand. Don’t let it change without your knowledge. And if you’re switched-test within a week. This isn’t about brand loyalty. It’s about survival. Lithium is one of the most effective drugs for preventing suicide in bipolar disorder. But only if you get the dose right. And with generics, that means paying attention to the details most people overlook.Can I switch between lithium generics without checking my blood levels?
No. Even if two generics are labeled the same, their absorption rates can differ enough to push your lithium level into the toxic range. Always get a blood test within 5-7 days of switching brands or formulations. This isn’t optional-it’s life-saving.
What’s the safest lithium level for long-term use?
For most adults on maintenance therapy, 0.6-0.8 mmol/L is the safest and most effective range. Higher levels (0.8-1.0 mmol/L) may be used for acute episodes but increase side effects like tremors, weight gain, and thyroid problems. For patients over 60, aim for 0.5-0.7 mmol/L due to reduced kidney function.
Why do some doctors still recommend 0.8-1.2 mmol/L?
Many doctors learned to use lithium in the 1980s or 1990s, when higher levels were standard. Back then, studies showed better mood control at 0.8-1.0 mmol/L. But newer data shows the same benefits at lower levels with far fewer side effects. The American Psychiatric Association updated its guidelines in 2021 to reflect this shift. Still, outdated practices persist in some clinics.
Are brand-name lithium products safer than generics?
Not necessarily. All FDA-approved generics must meet bioequivalence standards. But brand-name products often have more consistent manufacturing, better documentation, and fewer formulation changes. The real risk comes from switching between generics. If you’re stable on a generic, stay on it. Don’t switch unless your doctor approves and you test your levels after.
Can I take ibuprofen or other painkillers while on lithium?
Avoid NSAIDs like ibuprofen, naproxen, or celecoxib. They reduce how fast your kidneys clear lithium, which can cause levels to spike dangerously-even if you’ve been stable for years. Use acetaminophen (Tylenol) instead for pain or fever. Always tell your doctor or pharmacist you’re on lithium before taking any new medication.
How often should I get my kidney and thyroid checked?
At least twice a year. Check serum creatinine, estimated glomerular filtration rate (eGFR), and thyroid-stimulating hormone (TSH). For better accuracy, ask for cystatin C instead of creatinine-it’s more reliable in older adults and people with low muscle mass. If your eGFR drops below 60 mL/min, your doctor should reassess your lithium dose.
Is lithium still worth using with all the newer drugs available?
Yes. Despite newer mood stabilizers, lithium remains the most effective drug for preventing suicide in bipolar disorder. Long-term studies show it reduces relapse rates by up to 70% and cuts suicide risk by over 80%. It’s also the only medication proven to reduce manic and depressive episodes equally well. The challenge isn’t effectiveness-it’s managing the monitoring. If you’re willing to stick with blood tests and checkups, lithium is still the gold standard.


10 Comments
I switched generics last year and didn’t check my levels. Ended up in the ER with tremors so bad I dropped my coffee. Took me months to feel normal again. Don’t be like me. Test after every switch. Period.
Also, my pharmacist didn’t even tell me they changed it. Just handed me a different bottle. That’s not service-that’s negligence.
Ugh, another one of these ‘lithium is magic but also death’ posts. Look, if you can’t handle a simple blood test, maybe you shouldn’t be on a drug that requires one. Stop blaming generics. Stop crying about side effects. Take responsibility.
Also, if you’re on lithium and still using ibuprofen? You’re not a patient-you’re a liability.
There’s a quiet revolution happening in psychopharmacology, and lithium is at the center of it. We’ve spent decades treating it like a relic, but the data’s clear: it’s still the most powerful suicide-prevention tool we have.
What’s changing isn’t the drug-it’s our understanding. The old 0.8–1.2 range? That was a blunt instrument. Now we know precision matters. Lower targets, better safety, same efficacy.
And yes-switching generics without testing is like changing your insulin brand without recalibrating your pump. It’s not just risky, it’s reckless. But here’s the hopeful part: the FDA’s new guidance means we’re finally forcing manufacturers to prove real-world equivalence, not just lab numbers. That’s progress.
For anyone reading this: you’re not being paranoid. You’re being smart. Keep asking questions. Keep demanding tests. Your brain is worth it.
EVERY GENERIC IS A GOVERNMENT PLOT. 🤫💊
Did you know the FDA gets paid by pharma companies to approve these? That’s why they let the 80–125% range even exist. They don’t care if you turn into a shaking zombie. They just want you to keep buying pills.
My cousin’s uncle’s neighbor took lithium and woke up in a psychiatric ward with a feeding tube. No one told him about the switch. It’s all connected. 🌐👁️
Also, I heard they put fluoride in the water to mask lithium toxicity. Don’t drink tap. Only bottled. And only from a trusted source. I have a spreadsheet.
While the clinical data presented in this post is both comprehensive and well-supported, it is imperative to underscore the ethical obligation of prescribers and pharmacists to ensure continuity of care when managing narrow therapeutic index medications.
As evidenced by the 2024 Journal of Psychopharmacology study, bioequivalence standards, while statistically valid, fail to account for inter-individual pharmacokinetic variability. The 80–125% absorption window, though technically compliant, represents a clinically significant margin for patients with marginal renal function or polypharmacy.
Therefore, it is not merely advisable but medically necessary to implement a protocol requiring explicit documentation of the manufacturer and formulation at every dispensing event, coupled with mandatory serum level monitoring within 72–96 hours of any substitution. This is not an inconvenience-it is a standard of care.
Furthermore, the integration of pharmacogenomic screening, particularly for CYP2D6 and SLC6A4 variants, should be considered in all new lithium initiations. The future of personalized psychiatry is not speculative-it is imminent.
Man, I wish I’d known all this when I started lithium five years ago. I was just happy to get the prescription filled, you know? Didn’t even know there were different kinds.
Now I’ve got my own little lithium notebook-brand, date, level, how I felt that day. I even take pics of the pill bottle before I swallow. Sounds weird? Maybe. But I’ve been stable for two years now, and I’m not going back to blind faith.
And yeah, I use Tylenol now. No more Advil. Even my mom gets it. She’s 71, on lithium too. We’re basically a lithium support group now. 😄
Don’t let the system make you feel crazy for caring. You’re not crazy-you’re awake.
People these days act like lithium is some fragile, mystical potion. It’s a salt. A simple, ancient, inorganic compound. If you can’t handle a little variation between generics, maybe you’re not mentally stable enough to be on it in the first place.
And don’t get me started on the ‘don’t substitute’ nonsense. That’s not patient empowerment-that’s enabling medical infantilization. If you can’t follow basic instructions like ‘get your blood drawn,’ you shouldn’t be trusted with a prescription at all.
Also, if you’re over 60 and still on lithium, you’re a walking time bomb. The kidneys don’t recover. Stop pretending aging isn’t a risk factor.
Stop coddling people. Start holding them accountable.
I just wanted to say thank you for writing this. I’ve been on lithium for 11 years. I’ve had two ER trips because of switches. I didn’t know I was supposed to ask for a blood test after. I thought it was just ‘check in every 6 months.’
Now I print out the pill bottle and keep it in my wallet. My doctor laughs, but I don’t care. I’m alive because I paid attention.
You’re not alone. I see you. 💙
Okay, so picture this: lithium is the Beyoncé of mood stabilizers-iconic, powerful, and if you mess with the choreography (i.e., switch generics), you’re gonna get a standing ovation… or a full-blown toxic meltdown.
And the FDA’s 80–125% bioequivalence window? That’s like saying two cars are ‘equivalent’ because one goes 0–60 in 6 seconds and the other in 10. Sure, both have wheels. But one’s a Tesla. The other’s a rusty lawn mower with a turbo.
Also, cystatin C? That’s the new black. Creatinine is so 2008. If your doc hasn’t mentioned it, ask. Loudly. With emojis. 🧠🩸🧪
And yes-your pharmacist is not your therapist. But they *are* your first line of defense. Don’t let them slide. Demand transparency. Be the annoying patient. You’ll thank yourself later.