Cumulative Drug Toxicity Calculator
Cumulative Exposure Results
Total Cumulative Dose:
0.0 mg
Risk Level:
LowNote: This calculator uses standard safety thresholds. Always consult your doctor for personalized medical advice.
Most people assume that if a medication is safe for a few weeks, it’s safe for years. But that’s not always true. Some drugs don’t hurt you right away - they wait. Slowly, quietly, they build up in your body until one day, you wake up with a cough you can’t shake, your skin turns yellow, or your heart starts skipping beats. This isn’t bad luck. It’s cumulative drug toxicity.
What Exactly Is Cumulative Drug Toxicity?
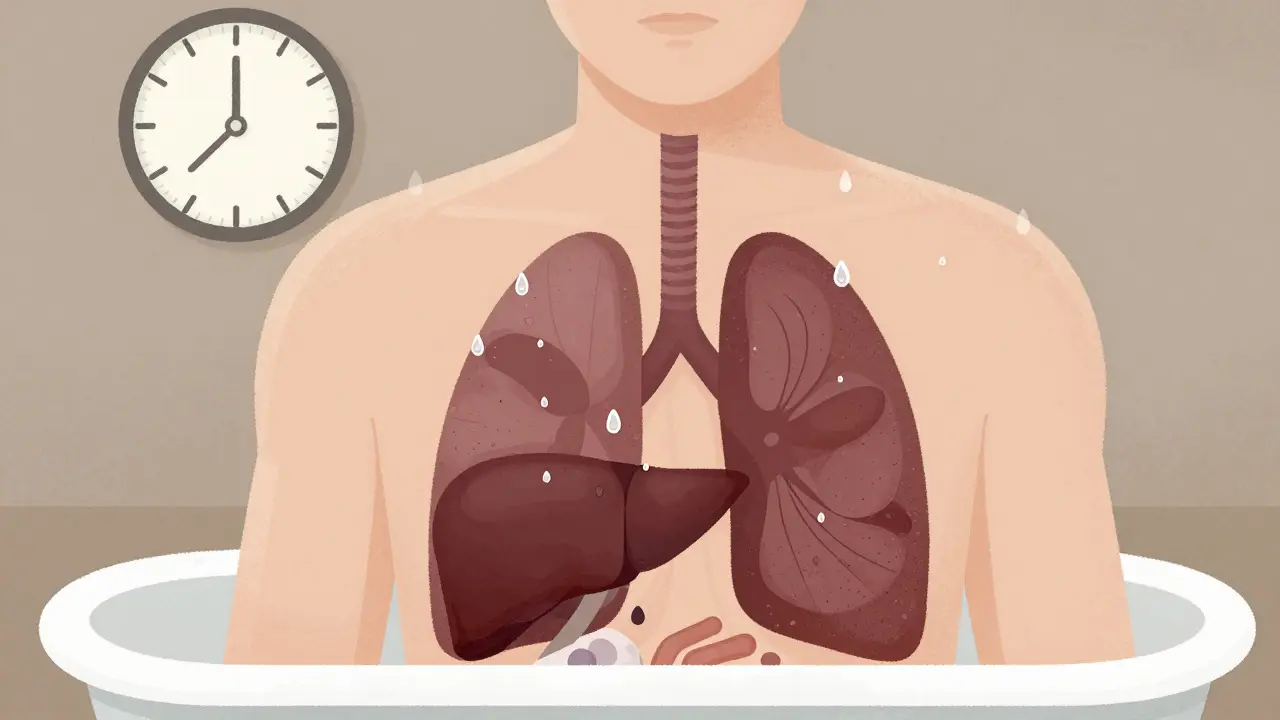
Cumulative drug toxicity happens when your body can’t get rid of a medicine fast enough. Every time you take a pill, a little bit stays behind. Over weeks, months, or even years, those leftovers pile up. Eventually, the amount in your system crosses a line - from therapeutic to toxic. It’s not an overdose. It’s a slow creep. Think of it like filling a bathtub with a slow leak. You don’t notice the water rising at first. But after a week, the floor is soaked. That’s what happens with drugs like amiodarone, digoxin, or methotrexate. They stick around. And the longer you take them, the more they accumulate. Drugs with long half-lives are the worst offenders. A half-life is how long it takes for half the drug to leave your body. If a drug has a half-life of 24 hours, it takes about five days to clear. But if it’s 10 days - like amiodarone - it can take months to fully wash out. That’s why someone on the same dose for five years might suddenly develop lung damage, even if their blood levels looked fine last month.Who’s Most at Risk?
It’s not just the elderly, though they’re hit hardest. About 68% of adverse drug reactions in older adults are tied to cumulative toxicity, according to the Journal of the National Cancer Institute. Why? Because as we age, our kidneys and liver slow down. They can’t filter drugs like they used to. A dose that was safe at 50 might be dangerous at 75. People with chronic conditions are also at higher risk. If you have kidney disease, liver cirrhosis, or heart failure, your body’s clearance rate drops by 30% to 50%. That means even standard doses can become toxic over time. And then there’s the silent factor: fat-soluble drugs. Vitamins A, D, E, and K, as well as heavy metals like lead and mercury, don’t dissolve in water. They hide in fat tissue and bone. Once stored, they can stay for months or even years. That’s why long-term use of vitamin A supplements can lead to liver damage - not from one big dose, but from years of small ones.Real Cases, Real Consequences
One oncologist on Reddit shared a case of a patient who’d been on amiodarone for arrhythmia for six years. Blood tests showed normal levels. No red flags. Then, out of nowhere, the patient developed severe pulmonary fibrosis. The cumulative dose? Over 600 grams. That’s more than most doctors even track. The FDA’s adverse event database shows over 12,000 reports of cumulative toxicity between 2018 and 2022. Nearly half involved blood thinners like warfarin. Another 28% were heart drugs like digoxin. These aren’t rare. They’re predictable - if you’re looking. In rheumatology clinics, methotrexate is a common treatment for arthritis. It’s cheap, effective, and usually safe. But if you take it for five years without monitoring liver enzymes or blood counts, you risk permanent scarring. One study found that clinics using a simple cumulative dose tracker reduced methotrexate-related hospital visits by 37%.
Why Don’t Doctors Catch This Sooner?
Because most of the time, they’re not looking. Standard blood tests check for immediate side effects - liver enzymes, kidney function, electrolytes. But they don’t track total exposure. A patient might have a normal digoxin level today, but if they’ve taken 500 doses over three years, their body is saturated. The test doesn’t show that. A 2022 Medscape survey found that 82% of doctors say patients miss follow-up appointments. That’s the biggest gap. People stop getting blood tests because they feel fine. But cumulative toxicity doesn’t care how you feel. It only cares about the total dose. And here’s the kicker: many drugs don’t even come with clear cumulative dose limits. You have to dig for them. For example, anthracycline chemotherapy drugs - used in breast cancer - have a lifetime limit of 450 mg/m² to avoid heart damage. That number comes from 17 studies involving 8,500 patients. But if your oncologist doesn’t know it, or doesn’t track it, you could easily cross that line without realizing.Which Medications Carry the Highest Risk?
The American Geriatrics Society Beers Criteria - a trusted guide for safe prescribing in older adults - lists 34 drugs with high cumulative toxicity risk. Here are the big ones:- Amiodarone - for irregular heartbeat. Can cause lung, liver, and thyroid damage after years of use.
- Digoxin - for heart failure. Builds up in the kidneys. Toxicity can cause nausea, confusion, and dangerous heart rhythms.
- Lithium - for bipolar disorder. Narrow safety margin. Even small drops in kidney function can push levels into danger.
- Methotrexate - for autoimmune diseases. Can cause liver fibrosis and bone marrow suppression over time.
- Aminoglycosides - antibiotics like gentamicin. Can permanently damage hearing and kidneys with prolonged use.
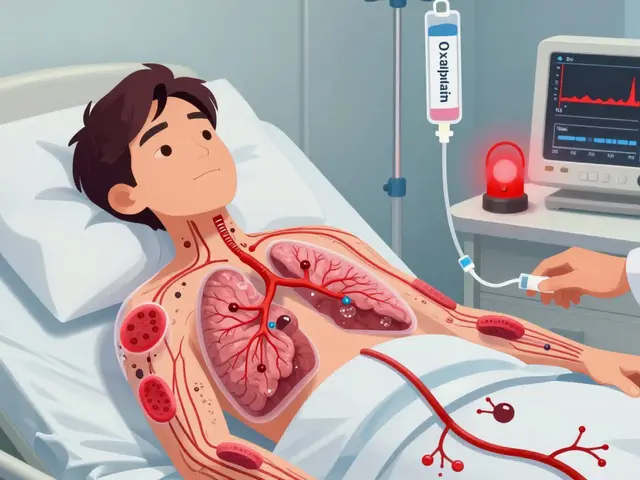
- Anthracyclines - cancer drugs like doxorubicin. Heart damage is irreversible and dose-dependent.
How to Protect Yourself
If you’re on long-term medication, here’s what to do:- Ask your doctor: “Is there a cumulative dose limit for this drug?” If they don’t know, ask for a referral to a pharmacist.
- Track your doses. Keep a log - even a simple spreadsheet. Note the name, dose, and start date. Many apps can help with this.
- Stick to monitoring. If you’re told to get blood tests every three months, don’t skip them. Even if you feel fine.
- Know your kidney and liver function. Ask for your latest eGFR (kidney) and ALT/AST (liver) numbers. A drop of 10% over six months matters.
- Don’t assume natural = safe. Herbal supplements like kava or comfrey can also build up and harm your liver. They’re not regulated like prescription drugs.
The Future Is Tracking - But It’s Not Everywhere Yet
The good news? The system is changing. In 2024, the European Medicines Agency made cumulative toxicity assessments mandatory for all new chronic-use drugs. The FDA now requires cumulative dose warnings on 78% of new oncology drugs - up from 52% in 2017. Some hospitals use AI to predict your risk. Memorial Sloan Kettering is testing models that analyze 27 factors - your age, weight, kidney function, genetics, even your diet - to forecast how much of a drug you’ll accumulate over time. It’s 82% accurate in trials. But here’s the reality: only 38% of electronic health records in the U.S. can automatically track cumulative doses. Most still rely on paper logs or memory. That’s why so many cases slip through.You’re Not Alone - But You Are Responsible
Cumulative toxicity isn’t a failure of medicine. It’s a failure of awareness. We’ve gotten so good at treating chronic disease that we forget: treating it for life means managing hidden risks. If you’ve been on the same medication for five years and feel fine - that’s great. But don’t assume it’s still safe. Ask the questions. Track the numbers. Push for monitoring. Because the next side effect you feel might not be from this week’s pill. It might be from the one you took five years ago - still hiding in your fat, waiting to wake up.Can cumulative drug toxicity be reversed?
It depends on the drug and how much damage has been done. For some, like lithium or digoxin, stopping the drug and letting your body clear it can reverse symptoms over weeks or months. But for others - like lung damage from amiodarone or heart damage from anthracyclines - the harm is often permanent. Early detection is key. The sooner you catch it, the better your chances of recovery.
Do over-the-counter supplements cause cumulative toxicity?
Yes. Fat-soluble vitamins like A, D, E, and K can build up in your body. High-dose vitamin A supplements over years can cause liver scarring. Too much vitamin D can lead to calcium deposits in your kidneys and blood vessels. Even herbal products like kava or comfrey have been linked to liver toxicity after long-term use. Just because something is sold as “natural” doesn’t mean it’s safe in large or prolonged doses.
Why don’t all doctors monitor cumulative doses?
Many don’t know the limits exist, or they assume standard blood tests are enough. Others don’t have the tools. Electronic health records rarely auto-calculate total doses. And time is tight - a 15-minute appointment isn’t enough to dig into 10 years of medication history. Pharmacists and specialized clinics are better equipped for this kind of tracking, which is why working with them can make a big difference.
Is cumulative toxicity only a problem for older people?
No. While older adults are more vulnerable due to slower metabolism, younger people on long-term meds - like those with autoimmune diseases, epilepsy, or chronic pain - are also at risk. People with genetic variations that affect liver enzymes (like CYP450) can accumulate drugs faster than average, regardless of age. It’s not about how old you are - it’s about how long you’ve been taking the drug and how your body handles it.
What should I do if I think I’m experiencing cumulative toxicity?
Don’t stop your medication on your own. Call your doctor or pharmacist. Write down your symptoms, when they started, and how long you’ve been on the drug. Bring your medication log. Ask specifically: “Could this be from cumulative buildup?” Request tests for organ function (liver, kidney, heart) and ask if your drug has a known cumulative limit. Early action can prevent permanent damage.



13 Comments