
If you’ve ever scrolled through your medicine cabinet looking for relief from swollen joints or an unruly gut, you might have run into a small, plain pill stamped with a mysterious name—Azulfidine. This drug doesn’t get the same spotlight as the flashy new biologics, but for people dealing with rheumatoid arthritis or ulcerative colitis, it’s a reliable sidekick they quietly depend on. You might be surprised to know it’s been around for nearly a century, and it’s still going strong—so clearly, Azulfidine, or sulfasalazine, must be doing something right.
What is Azulfidine and How Does it Work?
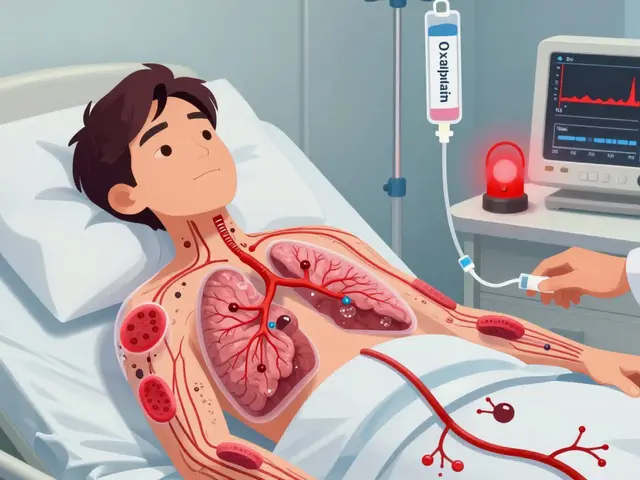
So what’s hidden inside Azulfidine’s tiny, orange shell? The answer: sulfasalazine. It’s a compound medicine, an old-school blend of a sulfa antibiotic and an anti-inflammatory cousin called 5-aminosalicylic acid. Originally whipped up back in the 1930s, it was designed to tackle bacterial infections and inflammation—kind of a double whammy. But the real magic happens after you swallow the pill. In your gut, friendly bacteria split sulfasalazine into its two active parts. The 5-aminosalicylic acid fights inflammation right at the heart of your colon, making it a lifesaver for people with ulcerative colitis, while the sulfa part tackles bacteria.
Doctors figured something out as the decades ticked on: Azulfidine doesn’t only calm angry guts—it also quiets the ruckus inside overactive immune systems. That’s why it earned a spot in the toolkit for rheumatoid arthritis. Studies have shown sulfasalazine slows joint damage, eases stiffness, and helps folks move better. It’s not a cure, but it takes the edge off for thousands with autoimmune issues. While the exact action still leaves scientists scratching their heads, the working theory is that it blocks chemicals like prostaglandins and cytokines that fuel inflammation. It’s like throwing a wet blanket over a fire without putting it out entirely.
You might be wondering: is this drug just for adults? Nope. Azulfidine is used for inflammatory bowel disease in both adults and children. There’s even a liquid form, which makes dosing easier for the little ones. Just a heads up, the pill has a reputation for smelling a bit like rotten eggs thanks to the sulfa part—no one takes it for the aroma. Doctors often start patients on a low dose and build up slowly to keep side effects at bay. It can take several weeks before you even start noticing results, so patience is key.
Common Uses and Practical Benefits of Azulfidine
Rheumatoid arthritis and ulcerative colitis are where Azulfidine truly shines. It’s also a fallback for Crohn’s disease, especially if the colon itself is inflamed. For arthritis, its use is typically as DMARD—that’s doctor-speak for disease-modifying antirheumatic drug. It’s not just masking symptoms but actually slowing the progression of joint damage over time. Some patients even combine sulfasalazine with other DMARDs like methotrexate to hit inflammation from different angles.
In ulcerative colitis and Crohn’s, the main win is getting off the rollercoaster of urgent bathroom visits and constant cramps. Azulfidine’s anti-inflammatory powers help reduce diarrhea, bleeding, and after a few weeks, bring real-life changes that mean you might not need to memorize the location of every public restroom on your commute. Newer medications do exist, of course—immunomodulators and biologics, with fancy price tags—but sulfasalazine keeps holding its own due to its affordability and robust track record.
Another fact: Azulfidine can sometimes be used in rare cases for conditions beyond arthritis or IBD, like ankylosing spondylitis or psoriatic arthritis. It has a sort of Swiss army knife rep in rheumatology circles—never the flashiest tool, but dependable in a pinch.
Here’s something practical: Physicians usually check your G6PD enzyme levels before starting Azulfidine, since those with a deficiency risk rare blood issues. And if you’re pregnant or planning to be, the conversation around Azulfidine gets nuanced. It’s often considered safer than some alternatives, but requires close doctor supervision. People prone to kidney issues or sulfa allergies need to steer clear, too. Azulfidine can even color your urine or sweat a faint orange, a harmless but shocking surprise if you’re not warned in advance. Pro tip: Don’t wear your favorite white shirt until you know how your body reacts!
The drug’s flexibility also means it can be finely tuned—doses get tweaked based on weight, kidney function, and how your body responds. Check out this table for a quick look at typical dosing:
| Condition | Starting Dose (adults) | Maintenance Dose | Notes |
|---|---|---|---|
| Rheumatoid Arthritis | 500 mg daily | 1,000 mg - 2,000 mg/day in divided doses | Build up slowly over weeks |
| Ulcerative Colitis | 500 mg - 1,000 mg 2-4x daily | 1,000 mg 4x daily | Adjust for severity and tolerance |
| Crohn's Colitis | Similar to UC | Similar to UC | Works best if colon affected |
| Children (IBD) | 40-60 mg/kg/day | Divided into 2-4 doses | Use liquid formula as needed |

Side Effects, Risks, and How to Manage Them
No one likes surprises when it comes to side effects. Azulfidine might seem mild compared to steroids or new wave biologics, but it’s not without baggage. Upset stomach, headache, and nausea are the most common complaints. That notorious sulfur smell has sent more than one patient racing for the breath mints. If you’re easily queasy, taking Azulfidine with food and a big glass of water helps. Your body does get used to it over time, so don’t throw in the towel after the first week.
Some folks notice a drop in appetite, or complain of mild dizziness. Periodically, people develop a low-grade fever or rash. The biggest concerns, though, are rare but serious: allergic reactions (especially for those with sulfa allergies), blood disorders, and liver or kidney problems. About 1 in 100 people see changes in their blood counts. That’s why regular check-ins and lab work matter—a quick blood draw every couple months keeps your doctor on top of things. They’ll be watching markers like white cell count, liver enzymes, and kidney function. Oh, and don’t be shocked if your urine turns yellow-orange. It’s a harmless quirk, but can be startling if you forget it’s coming.
If you’re the type to forget pills, set a daily reminder. Missing doses drops the drug’s effectiveness, especially with arthritis: consistency is key. One clever hack: leave your pills near your toothbrush or coffee mug to make taking them part of your daily ritual. Another overlooked side effect is sun sensitivity—a day at the pool can turn you lobster-red in no time. Slather on a high-SPF sunscreen, don a wide hat, and seek the shade. Wearing sunglasses isn’t overkill either, as Azulfidine can even irritate your eyes under bright light.
For those juggling other medications, tell your doctor about all supplements and prescriptions. Azulfidine can bump up the effects of anticoagulants (like warfarin) and lower levels of folate, a crucial B vitamin. Some doctors recommend taking a daily folic acid supplement—especially for women of childbearing age. You might notice blue pee if you’re taking methylene blue, another odd interaction. Remarkably, alcohol doesn’t usually interact much with Azulfidine, though it might worsen stomach side effects. Moderation is the way to go.
Here’s an interesting tidbit: up to 30% of patients never tolerate Azulfidine long term, mostly due to nausea or rashes. But for those who stick it out, studies from the past decade confirm a solid reduction in flare-ups and joint destruction—especially when combined with good diet, exercise, and anti-inflammatory habits. If you get sick of the smell or taste, ask your pharmacist for enteric-coated tablets which can be easier to swallow and less pungent in the stomach.
Tips for Living Well with Azulfidine
Managing chronic illness is more than taking a pill—it’s about building routines that help your body handle what comes next. Set up a calendar for regular lab work and jot down any new symptoms, no matter how minor. Doctors appreciate detailed notes, and it helps you advocate for yourself if you ever need to tweak your dose. Make hydration a daily goal: Azulfidine works better when you’re drinking plenty of water, and it helps keep kidneys happy. Treat your digestive tract kindly; avoid heavy, greasy foods and listen to your gut when it acts up.
No one gets excited for lifestyle changes, but ask anyone living with arthritis or IBD—they’ll tell you: exercise, sleep, and stress management make medications like Azulfidine work even harder. If you’re tempted to ditch meds on tough days, try linking progress with something enjoyable—track symptom-free streaks and reward yourself. Some people keep a symptom journal or use apps to track flares, foods, and pill routines. If you’re forgetful after a busy day (who isn’t?), those little alerts on your phone can save you from an accidental skip.
Feel free to tell friends and family about your treatment, especially when eating out or traveling. The orange pee and occasional upset stomachs don’t need to become embarrassing stories—just practical facts. Pack extra pills in your carry-on, bring a doctor’s note if crossing borders, and carry a list of your meds in your wallet. If your joints hurt, use heat packs or gentle stretching; for gut flares, some folks swear by bland diets, probiotics, or stress reduction—whatever works for you is right. Remember, no two bodies react the exact same way to Azulfidine. Stay patient and don’t be afraid to ask your medical team questions you find yourself Googling at 2am.
There’s a common myth that old medicines are less effective than newer options. The truth is, while Azulfidine may require more monitoring, it still punches above its weight when it comes to reducing hospital visits and flares. Costs stay lower, too—important when insurance battles are part of your life. The trick is sticking with regular appointments and not giving up over minor hiccups. If it’s not working for you, plenty of alternative therapies exist, but don’t jump ship without talking to your care team. In the world of IBD and arthritis, steady and informed wins the race more often than not.
Here’s a quick checklist for making Azulfidine part of your healthy routine:
- Take with food and lots of water.
- Use reminders or phone alerts.
- Avoid sun exposure and use sunscreen.
- Have regular blood tests as scheduled.
- Report side effects early—don’t tough them out in silence.
- Stay hydrated and eat a balanced diet.
- Know your triggers and avoid unnecessary stress on busy or tough days.
- Inform your care team about any other meds or supplements.
If there’s a golden rule with Azulfidine, it’s this: be proactive, ask questions, and don’t settle for misery. Modern medicine is a team sport, and Azulfidine works best when you and your doctor play it together.


9 Comments
Consider, if you will, the elegant paradox of Azulfidine: a molecule that is simultaneously a sulfa‑antibiotic and an anti‑inflammatory, a relic of the 1930s yet a mainstay of modern rheumatology; this duality invites reflection upon the nature of therapeutic compromise, where efficacy and side‑effects co‑exist in a delicate balance, and the clinician must navigate that terrain with both scientific rigor and, dare I say, philosophical humility.
While your exhaustive overview is commendably thorough, let us not overlook the simple truth: patients often abandon a drug not because of its pharmacology but due to the inconvenience of orange‑tinged urine-a fact that, frankly, could be avoided with a modest dose of empathetic counseling; consequently, I encourage practitioners to integrate a brief, yet highly formal, discussion on cosmetic side‑effects into every initial prescription, thereby preempting unnecessary discontinuation.
One might argue that the very act of dissecting sulfasalazine's mechanism borders on philosophical speculation, yet in practice the key takeaway is simple: split the dose, take with food, monitor labs. So, for those of us who enjoy a good chat over a pint, remember that the drug’s efficacy hinges on gut flora doing its job-no need for quantum physics. Keep it practical, keep it consistent.
Honestly this drug sounds like a drama queen you can't ignore and yet it's just a pill that smells like rotten eggs
Hey friends, let’s celebrate the unsung hero that is Azulfidine-yes, the orange tablet that refuses to be a TikTok star but quietly saves joints and guts! First off, take it with a hearty breakfast; a bowl of oatmeal or a smoothie works wonders and masks that notorious sulfur aroma. Second, keep a water bottle handy; staying hydrated not only eases the pill’s journey but also protects your kidneys, the often‑overlooked sidekick in this therapy. Third, set a phone alarm-trust me, forgetting a dose feels like losing a game of chess when you’re a grandmaster. Fourth, don’t shy away from asking your doctor about folic acid supplements; they’re cheap, effective, and can prevent that pesky anemia that sometimes sneaks up. Fifth, if you notice your urine turning a cheerful orange, wear that as a badge of honor-your body is simply saying, “I’m working!” Sixth, remember to schedule blood work every two to three months; those labs are the gossip columns of your health, spilling the tea on white cells and liver enzymes. Seventh, protect yourself from the sun-yes, the drug can make you a lobster, so slather on SPF 30 or higher, and consider a wide‑brimmed hat. Eighth, if the pill’s taste bothers you, ask your pharmacist about enteric‑coated versions; they’re smoother, less pungent, and just as effective. Ninth, celebrate small victories: a day without joint pain, a morning without urgent bathroom trips, a night of uninterrupted sleep-these moments add up like a mosaic of well‑being. Tenth, community matters; join a local or online support group, swap tips, and find solidarity in shared experiences. Eleventh, keep a simple symptom journal-just a notebook or an app can reveal patterns you’d otherwise miss. Twelfth, stay active with low‑impact exercises like swimming or yoga; movement lubricates joints and keeps the gut happy. Thirteenth, be kind to your mental health; chronic illness can be a heavy burden, and laughter truly is the best medicine alongside your prescription. Fourteenth, when you travel, pack extra pills and a doctor’s note; border checks love paperwork as much as they love stories. Fifteenth, finally, trust the process-Azulfidine may take weeks to show its full benefits, but patience combined with proactive care often yields the best outcomes. Keep shining, stay resilient, and remember: you’re not alone in this orange‑tinged adventure!
Great tips! Just remember to defnitely take it with food to avoid stomach upset.
Feeling so seen
While the author extols Azulfidine as a “reliable sidekick,” one must concede that the drug's reliance on gut bacteria for activation is a double‑edged sword; indeed, recent meta‑analyses suggest that in microbiome‑altered patients, efficacy drops dramatically-an observation conveniently omitted from the otherwise glowing narrative. Moreover, the claim of affordability ignores the hidden costs of regular laboratory monitoring, which can erode any price advantage. In sum, the pill is not the panacea some would have you believe.
Frankly, the whole “hidden costs” argument is a classic left‑wing exaggeration; in a truly competitive pharmaceutical market-unlike the monopolistic corridors we see in other nations-Azulfidine remains the cost‑effective choice for American patients who demand value without bowing to foreign regulatory overreach.