Pulmonary Fibrosis: What It Is and Why It Matters
When talking about pulmonary fibrosis, a progressive scarring of the lung tissue that makes breathing increasingly difficult. Also known as lung fibrosis, it belongs to the broader group of interstitial lung disease, disorders that affect the tissue and space around the air sacs of the lungs. The most common form, idiopathic pulmonary fibrosis, means the cause is unknown and it typically strikes people in their 60s or 70s. Understanding these connections is key because pulmonary fibrosis doesn’t happen in isolation – it intertwines with risk factors, diagnostic tools, and treatment choices.
How the Disease Develops and Who Is at Risk
Doctors explain that pulmonary fibrosis encompasses a cycle of lung injury, abnormal repair, and relentless scarring. Common triggers include long‑term exposure to silica dust, asbestos, or metal fumes, as well as certain medications like amiodarone or chemotherapy agents. Autoimmune conditions such as rheumatoid arthritis or scleroderma also raise the odds. When the lungs’ delicate alveoli become thickened, oxygen exchange drops, leading to shortness of breath, dry cough, and fatigue. Because the symptoms mimic asthma or chronic bronchitis, patients often receive a delayed diagnosis.
Diagnosis requires a mix of tools. High‑resolution CT scans reveal the hallmark honeycomb patterns, while pulmonary function tests quantify how much the lungs have lost capacity. In ambiguous cases, a lung biopsy may be performed to confirm the presence of fibrotic tissue. Early detection matters: the faster the disease is identified, the sooner interventions like anti‑fibrotic medication can slow progression.
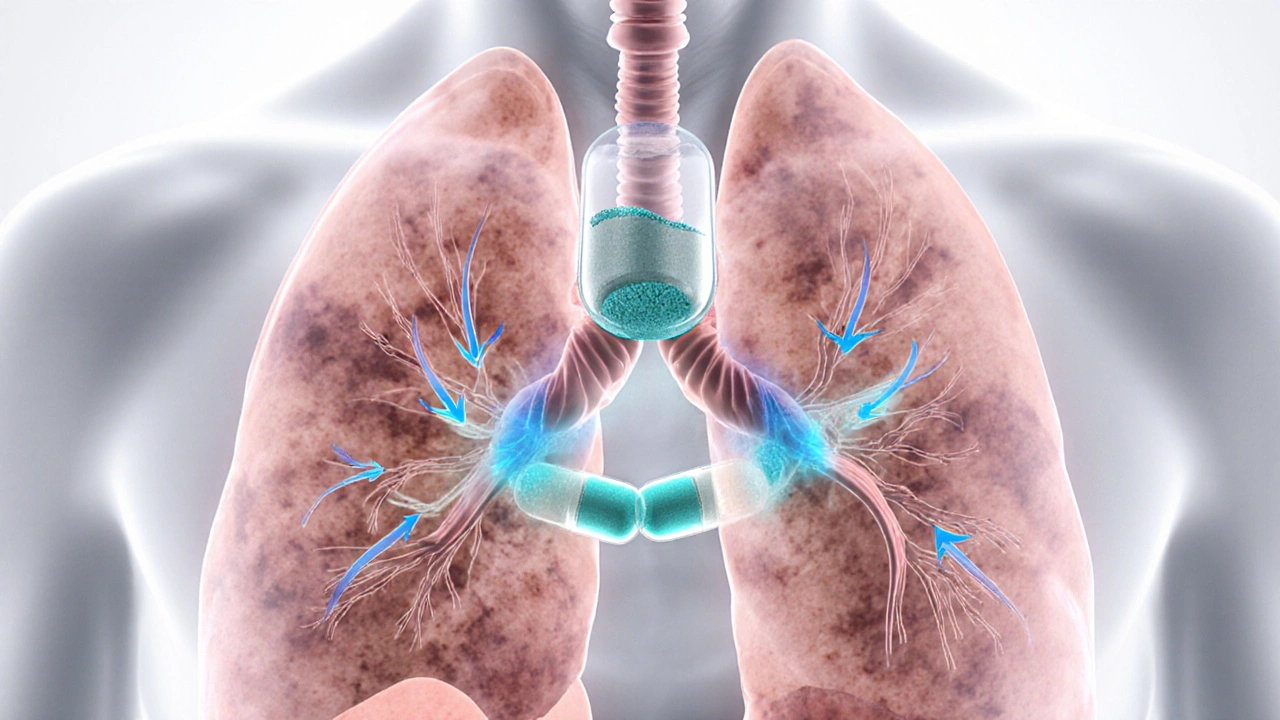
Speaking of treatment, the landscape has changed in the past decade. Anti‑fibrotic therapy, drugs such as nintedanib and pirfenidone that target the pathways leading to scar formation is now the frontline approach for most patients. While these medicines don’t cure the disease, they can reduce the rate of lung function decline and improve quality of life. Complementary measures include pulmonary rehabilitation, which combines exercise, breathing techniques, and education to boost stamina, and supplemental oxygen for those whose blood oxygen levels fall below safe thresholds.
When fibrosis advances to end‑stage disease, a lung transplant, the surgical replacement of diseased lungs with healthy donor organs becomes a viable option. Transplant candidates undergo rigorous screening, and post‑operative care involves lifelong immunosuppression and regular monitoring. Although not every patient qualifies, the procedure can extend survival dramatically and restore a level of normalcy that medication alone cannot achieve.
Beyond medical care, lifestyle adjustments play a supportive role. Quitting smoking, avoiding pollutants, maintaining a balanced diet, and staying active within individual limits all help manage symptoms. Mental health shouldn’t be overlooked either; chronic breathlessness often leads to anxiety or depression, so counseling or support groups can be valuable resources.
All of these pieces—risk factors, diagnostic methods, anti‑fibrotic drugs, rehab programs, and transplant possibilities—form the ecosystem around pulmonary fibrosis. In the list below you’ll find articles that dive deeper into each area, from practical buying guides for related medications to explanations of how other health conditions intersect with lung health. Use them as a roadmap to understand your condition better, make informed decisions, and connect with the right specialists.
Pirfenex vs Other IPF Drugs: In‑Depth Comparison Guide
A comprehensive comparison of Pirfenex (pirfenidone) with its main alternatives, covering efficacy, safety, cost, and practical tips for patients with idiopathic pulmonary fibrosis.
view more




