HFpEF: Understanding Heart Failure with Preserved Ejection Fraction and How Medications Affect It
When your heart can pump blood out fine but can’t fill up properly, you’re dealing with HFpEF, a form of heart failure where the left ventricle stiffens and doesn’t relax enough to fill with blood. Also known as diastolic heart failure, it’s not about weak pumping—it’s about stiff walls. This is the most common type of heart failure in older adults, especially women and people with high blood pressure, diabetes, or obesity. Unlike other heart failure types, EF (ejection fraction) numbers look normal on an echo, which makes it easy to miss—until you’re gasping after walking to the mailbox.
HFpEF doesn’t just sit there. It’s shaped by what you take. Diuretics, drugs that flush out extra fluid to ease swelling and shortness of breath are often the first line of defense. But they’re a double-edged sword—too much can drop your blood pressure too low, especially if you’re also on beta-blockers, medications like Toprol XL that slow your heart rate and reduce strain. That’s why lab monitoring calendars matter. You can’t guess your electrolytes or kidney function—you need blood tests on schedule. And then there’s GLP-1 agents, like Rybelsus, originally for diabetes but now showing promise in reducing heart failure hospitalizations. They don’t fix stiffness, but they help with weight, inflammation, and blood sugar—all drivers of HFpEF.
What you’re seeing in the posts below isn’t random. It’s a map of how real-world meds interact with this quiet, stubborn condition. You’ll find how diuretics raise heat risk, how beta-blockers compare when switching, how kidney changes in older adults force dose tweaks, and how gut bacteria might even alter how your body handles these drugs. No fluff. No theory without practice. Just what works, what doesn’t, and what you need to watch for—because HFpEF doesn’t announce itself. It sneaks in. And the right info? It can help you take back control.
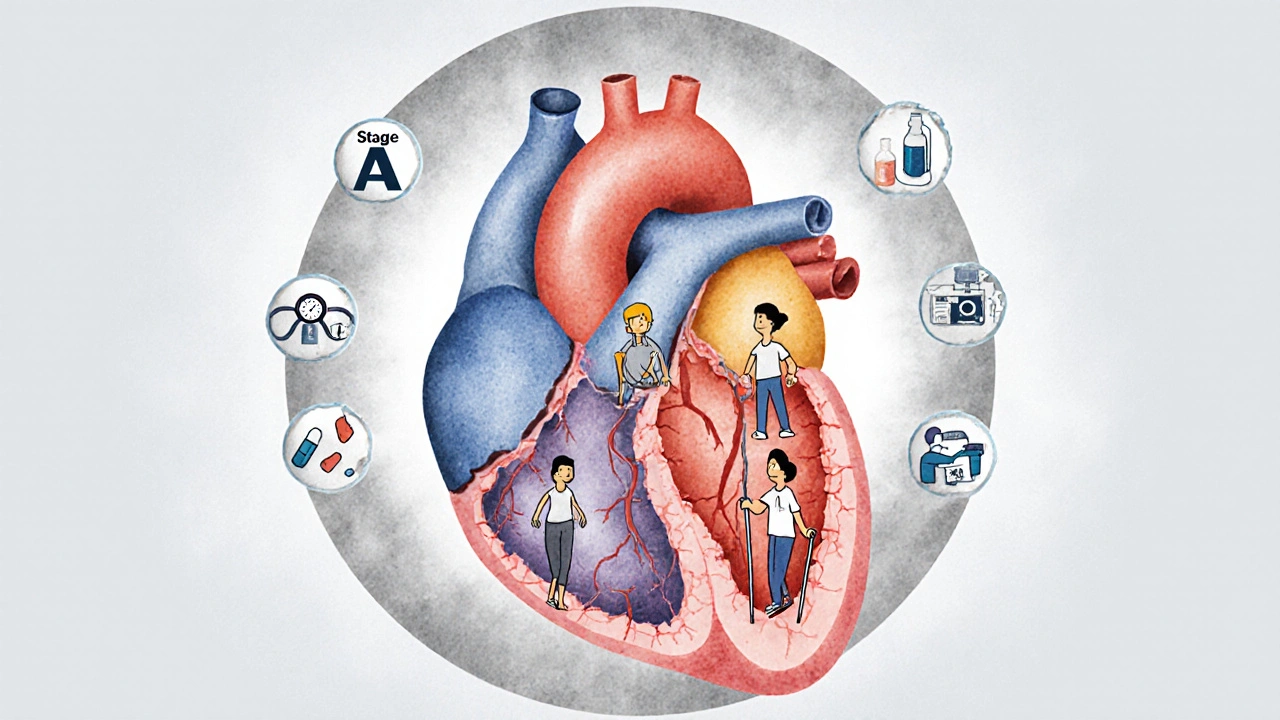
Heart Failure Management: From Diagnosis to Living Well
Heart failure management has changed dramatically. With new drugs like SGLT2 inhibitors and advanced monitoring tools, patients are living longer and better than ever. Learn how diagnosis, treatment, and daily care have evolved.
view more




