Steroid Injection Risk Calculator
Personal Injection History
Your Risk Assessment
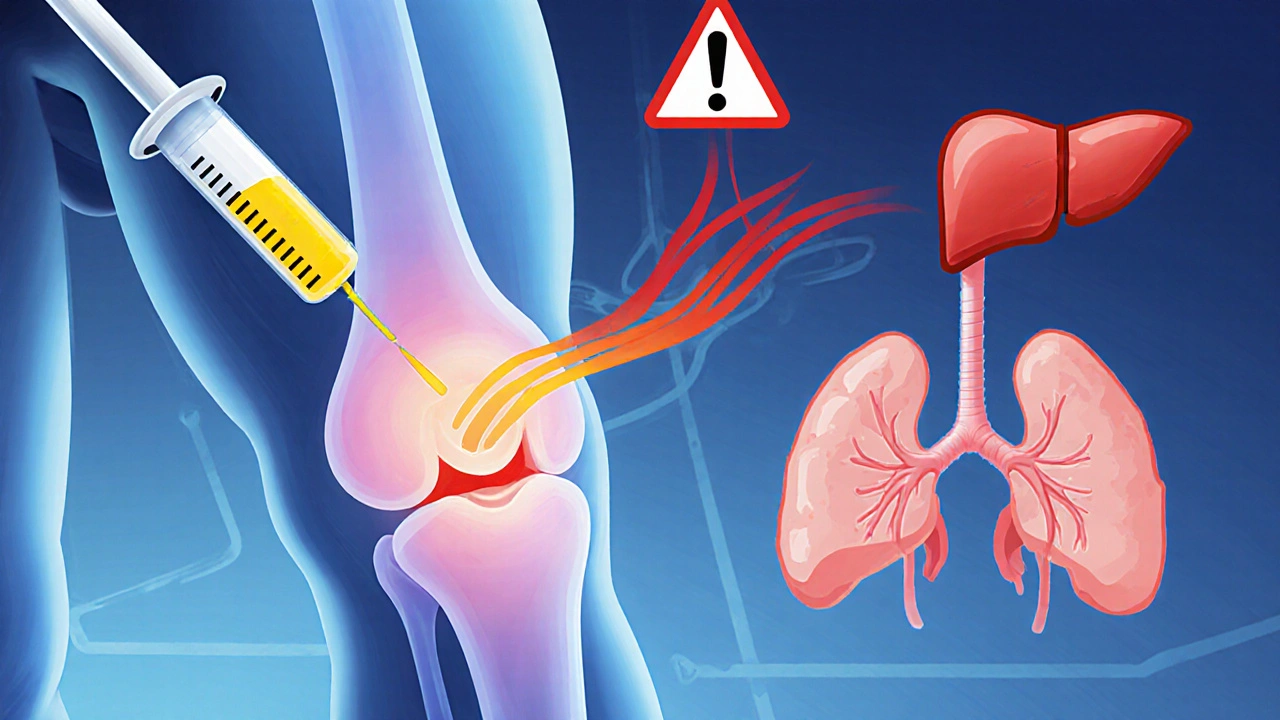
When your knee or hip hurts so badly that walking is a chore, a steroid injection can feel like a lifeline. Many people get them-about 12 million in the U.S. every year. Doctors offer them because they work fast: pain often drops within days. But here’s something most patients don’t hear until it’s too late: intra-articular steroid injections aren’t harmless. They can leak into your bloodstream, and what happens next might be worse than the pain you came in to fix.
How Steroid Injections Really Work (And Why They Leak)
The idea is simple: inject a powerful anti-inflammatory drug-like triamcinolone or methylprednisolone-directly into the joint. The goal is to shut down inflammation right where it’s hurting, without affecting the rest of your body. Sounds perfect, right? But joints aren’t sealed containers. Fluid moves in and out. Steroids do too. Studies show that even when the injection is perfectly placed, up to 30% of the dose can enter your bloodstream. Triamcinolone acetonide, one of the most common types, is especially prone to this. Once it’s in your blood, it acts like an oral steroid. That means it doesn’t just sit in your knee. It travels to your liver, your pancreas, your bones, your adrenal glands. And it doesn’t disappear after a day. Effects can linger for weeks.The Hidden Risks: More Than Just a Flare-Up
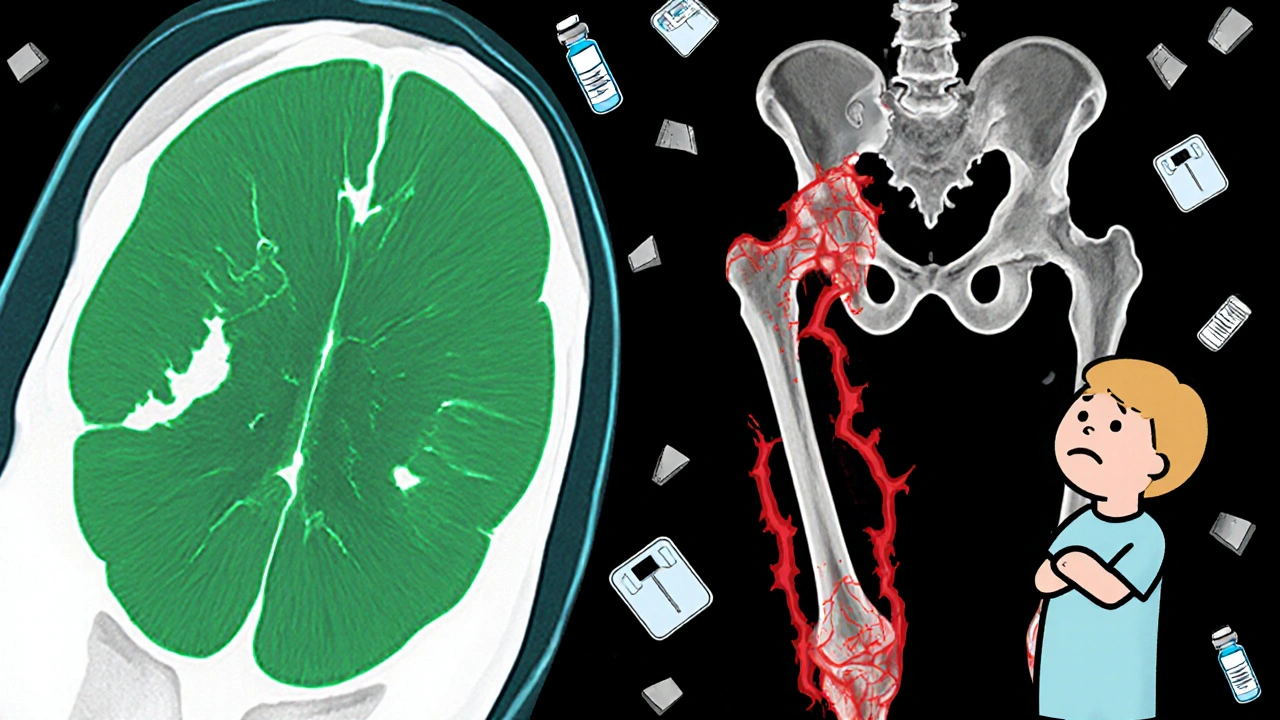
Most patients know about the short-term stuff-the temporary flare-up of pain after the shot, the redness or swelling at the injection site. But the real dangers are quieter, slower, and often invisible until it’s too late.- Accelerated joint damage: A 2023 study in Radiology followed patients after knee and hip injections. Those who got steroid shots were 3.2 times more likely to show visible joint space narrowing on X-rays over 12 months. For those getting multiple shots? The risk jumped to nearly 5 times higher. This isn’t just wear and tear-it’s accelerated destruction.
- Subchondral fractures: These are tiny stress fractures under the cartilage. They happen when bone weakens from steroid exposure. You won’t feel them coming. They show up on MRI as sudden, unexplained pain spikes.
- Osteonecrosis: Bone tissue dies. This is rare, but real. One study of 1,000 patients found a 1% combined rate of osteonecrosis, fractures, and rapid joint breakdown after steroid injections. For someone in their 50s with early osteoarthritis, that’s a real gamble.
- Blood sugar spikes: If you have diabetes-or even prediabetes-steroid injections can send your glucose levels soaring. One patient I know had to start insulin after a single knee shot. His levels stayed high for three weeks.
- Adrenal suppression: Your body makes cortisol naturally. Steroid shots tell your adrenal glands to stop. If you get too many, your body forgets how to make its own. That can lead to fatigue, low blood pressure, and even life-threatening crashes during illness or surgery.
Who’s Most at Risk?
Not everyone reacts the same. Some people get away with multiple injections. Others break down after one. Here’s who should be extra careful:- People with diabetes: Even one injection can wreck blood sugar control for weeks.
- Postmenopausal women: Bone density drops naturally after menopause. Steroids make it worse.
- Those with mild osteoarthritis: If your X-ray shows little damage but you’re in a lot of pain, the problem might not be the joint. It could be nerve irritation, inflammation elsewhere, or even a hidden stress fracture. Steroids won’t fix that-and they might make it worse.
- People planning surgery: If you’re thinking about a knee or hip replacement, steroid shots in the year before can increase infection risk and delay healing.
The Numbers Don’t Lie
Let’s put this in perspective. A 2023 analysis of data from the Osteoarthritis Initiative showed:- Patients who got one knee injection had a 3.2 times higher chance of joint space narrowing on X-ray.
- Those who got two or more had a 4.67 times higher chance.
- For hip injections, 44% of patients showed measurable joint space loss within six months.
But Some Studies Say It’s Safe-Why the Confusion?
You’ve probably heard that steroid injections are “safe and effective.” That’s not wrong-but it’s incomplete. Some studies say no harm. Others say major damage. Why the clash? It comes down to what’s being measured. Some studies look at pain relief. Others look at joint structure. One trial by Dr. Raynauld found no change in joint space narrowing on X-rays. But another, led by Dr. Ali Guermazi, used MRI and found cartilage loss and bone marrow changes that X-rays miss. The truth? Pain can improve while the joint is still being damaged. The American Academy of Orthopaedic Surgeons still recommends steroid injections for knee osteoarthritis. But they say “conditionally”-meaning the benefits must outweigh the risks. That’s the key. Not all patients are the same. Not all joints are the same.What’s the Safe Limit?
Most guidelines say: no more than 3 to 4 injections per joint per year. But that’s a rough guess. The real limit? It’s personal. Think of it like this: each injection adds to your total steroid burden. If you’re also taking oral steroids for another condition-say, rheumatoid arthritis or lupus-that dose counts too. A 40 mg shot of triamcinolone is roughly equal to 10 mg of prednisone. If you’ve had two shots this year and you’re on 5 mg of prednisone daily, your total steroid exposure is higher than most doctors realize. There’s no blood test to measure cumulative exposure. But if you’ve had more than 3 injections in a year, especially in the same joint, you should ask: Is this helping, or just delaying the inevitable?
What Are the Alternatives?
If steroid shots carry hidden risks, what else works?- Physical therapy: Stronger muscles around the joint reduce stress. Studies show PT is as effective as injections for knee osteoarthritis-and it lasts longer.
- Weight loss: Losing just 10 pounds cuts knee pain by 50% in overweight patients. It’s the most powerful treatment no one talks about.
- Bracing and footwear: A simple knee unloader brace or cushioned shoe can shift pressure off damaged areas.
- Platelet-rich plasma (PRP) or hyaluronic acid: These are still being studied, but they don’t carry the same bone-damaging risks. PRP may even help repair tissue.
- Low-dose NSAIDs: For short-term use, they can help without systemic steroid effects.
What Should You Do?
If you’re considering a steroid injection:- Ask for an up-to-date X-ray or MRI. If your joint looks mostly healthy, ask why you need a shot.
- Ask your doctor: “Could this injection make my joint worse over time?”
- Get your blood sugar checked before and after if you have diabetes or prediabetes.
- Track how many injections you’ve had in each joint over the last year.
- Try PT, weight management, or bracing first. If nothing else works, then consider the shot.
- Never get more than one injection in the same joint within 3 months.
The Bottom Line
Steroid injections aren’t evil. They’re a tool. But like any tool, they can be misused. For older patients with advanced osteoarthritis and no other options, they can be a lifeline. But for younger people, or those with mild symptoms, they might be a trap. The goal isn’t just to reduce pain. It’s to keep your joints working for decades. One shot might give you a few months of relief. But if it speeds up joint failure, you’re paying for that comfort with your future mobility. Ask yourself: Am I treating the pain-or just hiding the problem?Do steroid joint injections cause weight gain?
Yes, but usually only with frequent or high-dose injections. Steroids increase appetite and cause fluid retention. Weight gain isn’t common after one or two shots, but it’s more likely if you’re getting multiple injections over months or have other risk factors like diabetes.
Can steroid injections cause diabetes?
They don’t cause diabetes directly, but they can trigger high blood sugar in people who are already at risk. If you have prediabetes or a family history of diabetes, a steroid injection could push you over the edge. Always check your blood sugar before and after.
How long do systemic side effects last after a steroid injection?
It depends on the type and dose. Triamcinolone can affect your blood sugar and adrenal system for up to 3-4 weeks. Facial flushing and mood changes usually fade in a few days. Bone density loss and cartilage damage, however, are long-term and may be irreversible.
Are there safer alternatives to steroid injections?
Yes. Physical therapy, weight loss, braces, and low-dose NSAIDs are often safer and just as effective for mild to moderate joint pain. PRP and hyaluronic acid injections carry less risk of joint damage, though they’re more expensive and not always covered by insurance.
Should I avoid steroid injections if I’m planning joint surgery?
Yes. Steroid injections within 6-12 months before joint replacement surgery increase the risk of infection and slow healing. Most surgeons won’t operate if you’ve had a steroid shot in that joint recently. Always tell your surgeon about every injection you’ve had.
Can steroid injections damage cartilage?
Yes. Multiple studies using MRI show that repeated steroid injections are linked to cartilage loss over time. This damage isn’t always visible on X-rays, but it’s real. The more injections you get, the higher the risk.
What’s the maximum number of steroid injections I should get in a year?
Most experts recommend no more than 3-4 injections per joint per year. But if you’re diabetic, postmenopausal, or have early osteoarthritis, even two may be too many. Always track your total dose and discuss your risk with your doctor.






10 Comments
Steroid injections are the pharmaceutical equivalent of putting duct tape on a leaking pipe and calling it a fix. You feel better for a few weeks, but the structure’s still crumbling underneath. I’ve seen patients come in with knees that look like they’ve been through a war-only to find out they’ve had six shots in two years. The pain was ‘managed.’ The joint? Dead on arrival.
Triamcinolone doesn’t just ‘leak’-it hijacks your endocrine system like a rogue AI. Your adrenals forget how to cortisol. Your bones start eating themselves. And don’t get me started on the blood sugar rollercoaster. One guy I knew went from prediabetic to insulin-dependent after a ‘simple’ knee shot. No one warned him. No one even asked if he had a history.
Doctors treat this like a vending machine: insert pain, get relief. But joints aren’t broken machines. They’re living, breathing ecosystems. You don’t pour bleach into a garden and expect the flowers to thrive. Yet we do this every day.
Physical therapy? Weight loss? Those are the real ‘long-term solutions.’ But they take effort. And effort doesn’t pay bills. Injections do. So the system keeps pushing them. And we keep paying the price in cartilage, bone, and insulin pens.
bro this is just fearmongering. i got 3 shots in my knee last year and i can now run again. who cares if my bones are ‘weakening’? im alive and pain free. doctors know what they doing. stop overthinking.
Just got my first shot last week. Felt amazing for 3 days. Then my blood sugar spiked like a rocket. Now I’m scared to get another. This post? Eye-opening. Thank you.
The fundamental fallacy in contemporary orthopedic practice lies in its ontological reductionism: the conflation of symptom suppression with therapeutic efficacy. One may achieve transient analgesia through exogenous glucocorticoid administration, yet the underlying pathophysiology-progressive chondrocyte apoptosis, subchondral bone remodeling, and microfracture accumulation-remains unaddressed, if not exacerbated.
Moreover, the epistemological blind spot of radiographic assessment-relying solely on X-ray joint space narrowing while ignoring MRI-demonstrated cartilage degradation and bone marrow edema-represents a profound epistemic failure. The patient experiences relief; the clinician declares success; the joint, however, continues its silent disintegration.
One must ask: Is medicine healing, or merely delaying the inevitable with pharmacological sedation? The ethical imperative demands that we prioritize structural preservation over momentary comfort, even when the latter is more readily marketable.
Physical therapy, though laborious and temporally demanding, constitutes the only intervention that simultaneously addresses biomechanical dysfunction and promotes tissue resilience. It is not a ‘alternative.’ It is the baseline standard of care, obscured by the seductive immediacy of the needle.
Let’s be clear: this isn’t medicine. It’s pharmaceutical sabotage disguised as care. Triamcinolone isn’t a treatment-it’s a Trojan horse. You think you’re fixing your knee? You’re actually seeding systemic chaos: adrenal fatigue, osteonecrosis, insulin resistance. And the AAO? They’re complicit. They’re paid by the same pharma giants pushing these injections. The data’s there. They just ignore it.
This is the new opioid crisis. Only instead of pills, it’s needles. And the addicts? They’re the ones who believe ‘it’s just one shot.’
One shot becomes two. Two becomes four. Four becomes a replacement joint at 52. That’s not medicine. That’s a business model.
They don’t want you to know this. The FDA, the AMA, the ortho docs-they’re all in on it. Steroid injections are a stealth weapon to push people toward joint replacements. Why? Because replacements are worth billions. You think they care if you walk for another 10 years? No. They want you on the operating table in 5.
They’re using steroids to destroy your cartilage slowly so you’ll need a $50k knee in 3 years. That’s the real agenda. They don’t want you to heal. They want you to upgrade.
And if you’re diabetic? Even better. More insulin prescriptions. More revenue. It’s all connected. Wake up.
OH MY GOD. I KNEW IT. I KNEW THEY WERE DOING THIS ON PURPOSE. I had two shots last year and now my hip feels like it’s crumbling. I thought it was just aging. Turns out? It’s a COVER-UP. The entire medical system is a pyramid scheme built on painkillers and implants. They don’t want you to move better-they want you to get replaced.
And don’t get me started on how they lie about ‘safe limits.’ 3-4 shots a year? LIES. I’ve had 7. I’m 49. I’m going to be on a walker by 55. And they told me it was ‘fine.’
They’re killing us slowly so they can sell us new parts. This isn’t healthcare. It’s corporate cannibalism.
Let’s cut the fluff. Steroid injections are a band-aid on a ruptured artery. You’re not treating osteoarthritis-you’re accelerating its progression. The data is unequivocal. MRI studies confirm cartilage loss. Bone marrow lesions. Subchondral collapse. These aren’t ‘side effects.’ They’re direct pharmacological consequences.
And yet, physicians continue to prescribe them like candy. Why? Because PT takes time. Weight loss requires discipline. Injections? Five minutes. Billable code 20610. Profit margin: 900%.
It’s not negligence. It’s incentivized malpractice. And if you’re postmenopausal or diabetic? You’re not a patient. You’re a revenue stream.
the truth is nobody gives a shit. doctors are overworked, patients want quick fixes, and insurance won’t pay for PT. so they give the shot. it’s not malice-it’s systemic collapse. the system is broken, not the medicine. we’re just the collateral.
also, the ‘alternatives’ are bullshit. who has time to go to PT 3x a week? who can lose 20lbs when they’re in pain? it’s a trap. the only real solution is surgery. and even that’s a gamble.
we’re all just waiting for the next shot.
AMERICA IS BEING DESTROYED BY PHARMA GREED. THEY’RE TURNING OUR JOINTS INTO SCRAP METAL SO THEY CAN SELL US NEW ONES FOR $100K. AND THE MEDIA? SILENT. THE DOCTORS? COMPlicit. THE GOVERNMENT? ASLEEP.
THIS ISN’T JUST ABOUT KNEES-IT’S ABOUT CONTROL. THEY WANT US WEAK. THEY WANT US DEPENDENT. THEY WANT US ON INSULIN, ON WALKERS, ON SURGERY LISTS. SO WE STAY QUIET. SO WE DON’T QUESTION. SO WE KEEP PAYING.
THEY’RE NOT DOCTORS. THEY’RE CORPORATE AGENTS. AND WE’RE THE CATTLE.
STOP THE INJECTIONS. START THE REVOLUTION.