Hyperkalemia Risk Assessment Tool
Your Medications
Health Factors
Risk Assessment Results
Your hyperkalemia risk is
Recommended Actions
Emergency Alert: If your potassium level exceeds 6.5 mEq/L or you experience heart palpitations, weakness, or shortness of breath, seek emergency medical care immediately.
Disclaimer: This tool is for informational purposes only. It is not a substitute for professional medical advice. Always consult your healthcare provider for personalized medical guidance.
When your blood potassium levels climb too high, your heart doesn’t just skip a beat-it can stop. This isn’t theoretical. Every year, thousands of people on common heart and kidney medications develop hyperkalemia, a silent but deadly spike in potassium that can trigger heart attacks, arrhythmias, and sudden death-often without warning. And here’s the twist: the very drugs meant to save your life can be the ones putting you at risk.
What Exactly Is Hyperkalemia?
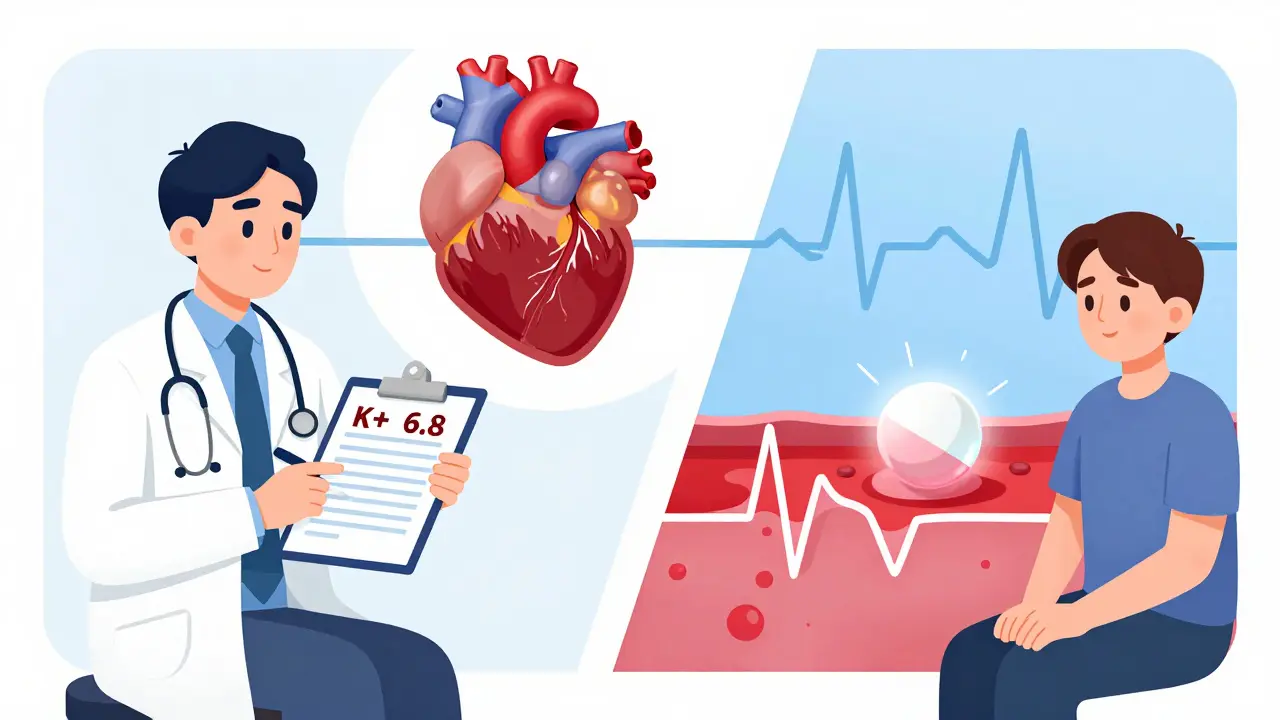
Hyperkalemia means your blood potassium is above 5.5 mEq/L. Normal levels sit between 3.5 and 5.0 mEq/L. At 6.5 mEq/L or higher, you’re in a medical emergency. Your heart’s electrical system starts to short-circuit. You might feel nothing at all-or you might feel your heart fluttering, get weak, or suddenly struggle to breathe. By the time symptoms show up, it’s often too late.
This isn’t rare. About 2-3% of the general population has it. But if you’re on blood pressure meds like lisinopril or losartan, or a diuretic like spironolactone, your risk jumps to 10-20%. For people with kidney disease or diabetes, it’s even higher. And because these conditions often go hand-in-hand, the problem is growing fast.
Which Medications Cause It?
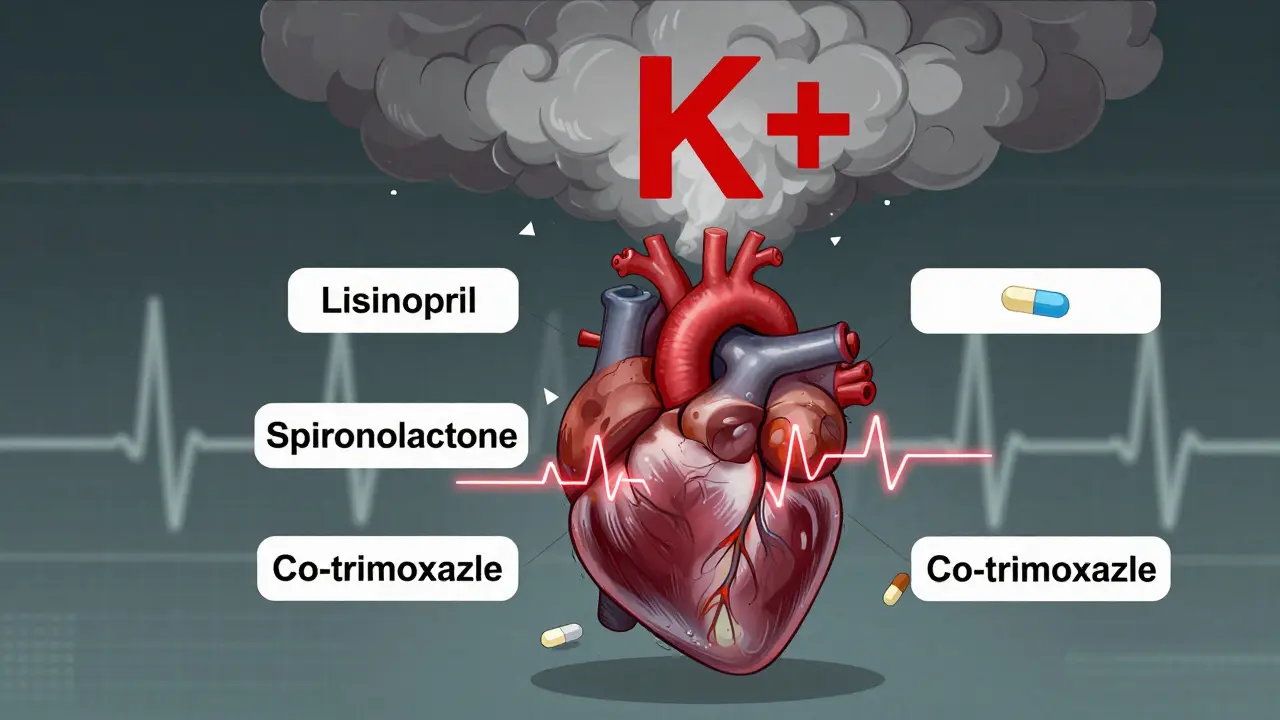
The biggest culprits are drugs that protect your heart and kidneys-but also block your body’s ability to flush out potassium. These include:
- ACE inhibitors (like lisinopril, enalapril)
- ARBs (like losartan, valsartan)
- Mineralocorticoid receptor antagonists (like spironolactone, eplerenone)
- Potassium-sparing diuretics (like amiloride, triamterene)
- Direct renin inhibitors (like aliskiren)
- Co-trimoxazole (an antibiotic sometimes prescribed for UTIs or lung infections)
Here’s the scary part: combining spironolactone with an ACE inhibitor or ARB, then adding co-trimoxazole, can make sudden death five and a half times more likely than using spironolactone alone. That’s not a typo. It’s a documented risk from Medsafe data.
How It Kills: The Heart’s Electrical Breakdown
Your heart beats because of tiny electrical signals. Potassium helps control those signals. Too much potassium makes your heart muscle cells too easy to trigger-and too hard to reset. This leads to chaotic rhythms.
At 5.5-6.5 mEq/L, you start seeing peaked T-waves on an ECG. At 6.5-7.5 mEq/L, the PR interval stretches out. Above 7.5 mEq/L, your QRS complex widens. If it hits 8.0 mEq/L or higher, you get a sine wave pattern-and then ventricular fibrillation. No pulse. No heartbeat. Death in minutes.
And here’s what most people don’t know: you can have all of this happen without feeling a thing. That’s why regular blood tests matter more than symptoms. If you’re on one of these meds, your doctor should check your potassium every 1-4 weeks, especially when starting, changing doses, or if you’re sick or dehydrated.
Why Doctors Are Stuck
These medications-ACE inhibitors, ARBs, spironolactone-are lifesavers. They cut heart failure deaths by up to 35%. They slow kidney damage in diabetics. Stopping them means trading one risk for another: better potassium levels, but higher chance of heart attack, stroke, or dialysis.
Back in 2015, nearly 4 out of 10 patients had to lower or stop their heart meds just because their potassium crept up a little. That’s not just inconvenient-it’s dangerous long-term. For years, doctors had no good solution. Either risk the heart or risk the potassium.
The New Game-Changer: Potassium Binders
Since 2015, two drugs have changed everything: patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma). These aren’t diuretics. They’re oral binders that grab excess potassium in your gut and flush it out in your stool.
Here’s what they do:
- Lower potassium by 0.4-1.0 mEq/L within hours
- Let you keep taking your heart and kidney meds
- Reduce the need to stop or downsize your treatment
A 2024 study showed that 86% of patients stayed on their full dose of RAAS inhibitors when using patiromer. Without it, only 66% could. That’s a massive difference in long-term survival.
They’re not perfect. About 15-20% of people get constipation. 10-15% get diarrhea. But compared to the risk of stopping your heart meds, that’s a fair trade.
What to Do in an Emergency
If your potassium hits 6.5 mEq/L or higher, or if your ECG shows changes, you need immediate treatment. It’s not a wait-and-see situation.
The first step? Calcium gluconate. Given IV, it doesn’t lower potassium-but it protects your heart within 2-3 minutes. It’s like putting a shield around your heart muscle while you work on removing the excess potassium.
Then come the drugs that shift potassium into your cells:
- Insulin + glucose: 10 units of insulin with 25g of glucose. Lowers potassium by 0.5-1.5 mEq/L in 15-30 minutes.
- Albuterol nebulizer: 50-100 mcg. Lowers potassium by 0.5-1.0 mEq/L.
After that, you need to get the potassium out of your body. That means stopping all potassium supplements, avoiding salt substitutes, and sometimes using loop diuretics like furosemide if your kidneys can still handle it.
Long-Term Management: Beyond the Emergency
If you’re on long-term RAAS therapy and have had hyperkalemia before, you need a plan:
- Get your potassium checked every 1-4 weeks, depending on stability.
- Consider a potassium binder if you’re on multiple risk-increasing meds.
- Watch your diet. Aim for 2,000-3,000 mg of potassium per day. That means cutting back on bananas, oranges, potatoes, spinach, tomatoes, and salt substitutes (which are full of potassium chloride).
- Stay hydrated. Dehydration is a silent trigger.
- Tell every doctor you see-including your dentist-that you’re on RAAS meds. Many antibiotics and NSAIDs can push potassium higher.
And here’s the hard truth: only 15-20% of patients get proper dietary counseling. Most don’t know that a single banana has 400 mg of potassium. That’s 10-20% of your daily limit. A cup of cooked spinach? Nearly 800 mg. You don’t need to eliminate them-but you need to know how much you’re eating.
What’s Next?
Doctors are shifting from seeing hyperkalemia as a reason to stop meds to seeing it as a condition to manage. The National Kidney Foundation now recommends potassium binders as first-line for patients who need to stay on RAAS therapy. That’s a huge change.
Research is already looking at next-gen binders with fewer side effects. Some are in trials right now. The goal? Make it so easy to control potassium that no one has to choose between heart protection and safety.
Right now, the tools exist. The knowledge exists. The problem is awareness. If you’re on blood pressure or heart failure meds-and especially if you have kidney disease or diabetes-ask your doctor: "Have you checked my potassium lately?" If they haven’t, push for it. This isn’t about being difficult. It’s about staying alive.
Don’t Wait for Symptoms
Hyperkalemia doesn’t knock. It sneaks in. One day your meds are working fine. The next, your heart is on the edge. You don’t need to feel bad to be in danger.
Know your meds. Know your numbers. Know your options. And don’t let fear of side effects make you stop the drugs that keep you alive. With the right monitoring and new treatments, you don’t have to choose anymore.






9 Comments
Just had my potassium checked last week after starting lisinopril - 5.6. My doctor didn’t mention it until I asked. This post scared me a little but also woke me up. I’m getting a binder prescribed next month. No more guessing.
Been on spironolactone for 8 years for heart failure. My potassium’s been stable since I started Lokelma. I don’t feel like a lab rat anymore. Just wish more docs knew about this stuff.
Just read this and immediately texted my mom who’s on losartan and eats bananas every morning 🍌😭
Too much info. I just take my pills and hope for the best.
Big Pharma doesn’t want you to know this. Why? Because binders cost money. Meanwhile, your doctor’s getting kickbacks from the drug reps pushing ACE inhibitors. They don’t care if you die - they care about their quarterly reports. The system is rigged.
It is of considerable importance to note that the pathophysiological cascade initiated by hyperkalemia, particularly in the context of RAAS inhibition, involves not only the depolarization of cardiac myocytes but also a significant alteration in the kinetics of sodium channels, which may precipitate conduction delays that are not always detectable via standard ECG parameters unless serial monitoring is performed with high temporal resolution.
As a nephrologist in India, I see this every week - patients on ARBs and diuretics, eating too many bananas, not getting tested. We don’t have binders here. Many just stop their meds. Their BP spikes. Their kidneys fail. This post is a lifeline. Please, if you’re reading this - get your K+ checked. Your heart doesn’t lie.
I used to think death came with a warning sign - chest pain, dizziness, gasping. But this? This is quiet. It’s the kind of death that happens because no one asked the right question. I’m going to ask my doctor tomorrow. Not because I’m scared. Because I want to live. And if this knowledge can save even one person… then sharing it matters.