Patient Adherence: Why People Stop Taking Medication and How to Fix It
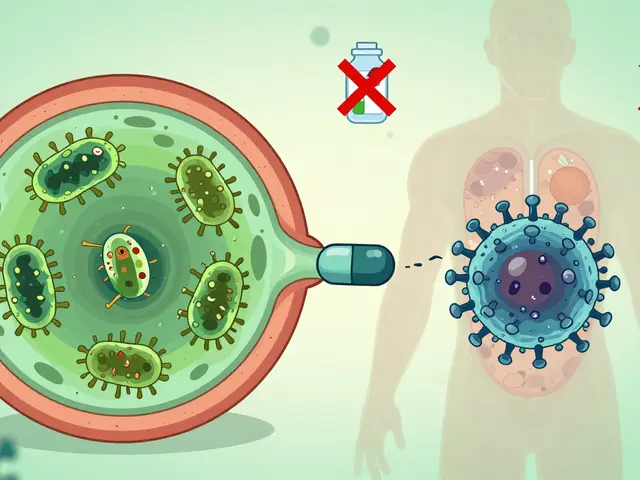
When someone stops taking their medicine even though it’s working, that’s not laziness—it’s a system failure. Patient adherence, the extent to which a person follows their prescribed treatment plan. Also known as medication compliance, it’s the quiet battle behind most hospital readmissions, worsening chronic conditions, and avoidable deaths. It’s not about willpower. It’s about confusion, fear, cost, and complexity.
Take health literacy, the ability to understand medical information and make informed health decisions. A lot of people quit generics because they think they’re "weaker" than brand names. They don’t know the FDA requires generics to work the same way. That misunderstanding isn’t rare—it’s common. And it’s deadly. Same with polypharmacy risk, the danger of taking too many drugs at once, especially for older adults. Five, six, even ten pills a day? It’s easy to mix them up, forget them, or not realize one is causing dizziness, confusion, or falls. No one tells you that a sleep aid and a blood pressure pill together can knock you out when you stand up.
Then there’s the side effects. drug side effects, unwanted reactions from medications that range from annoying to life-threatening, are often downplayed. A dry cough from an ACE inhibitor? A patient thinks, "This isn’t normal," and quits. A shaky hand from a beta-blocker? They assume it’s aging. They don’t call their doctor. They just stop. And when they do, their blood pressure spikes, their heart struggles, their kidneys get damaged. No one’s checking in. No one’s asking if the meds are working—or if they’re causing more harm than good.
This isn’t about blaming patients. It’s about fixing the gaps. The system doesn’t track whether someone took their pill. It doesn’t explain why a cheaper version is just as good. It doesn’t warn you that your new cholesterol drug might cause tendon tears or gout. And it sure doesn’t give you a calendar for blood tests you need to catch those risks early.
What works? Simple things. Clear instructions. Regular check-ins. Knowing what to watch for. Understanding that your gut bacteria might be turning your drug into something dangerous. Realizing that what you think is a penicillin allergy might just be a rash that went away. And learning that taking fewer pills—smartly combined—can be safer than taking more.
Below, you’ll find real, no-fluff guides that show exactly where patient adherence breaks down—and how to fix it. From spotting dangerous drug combos to understanding why generics are just as strong, these posts don’t just explain the problem. They give you the tools to solve it.

Multicultural Perspectives on Generics: How Culture Shapes Patient Trust and Adherence
Cultural beliefs about pill appearance, ingredients like gelatin, and trust in healthcare shape how patients use generic medications. Learn how religion, color, and misinformation affect adherence - and what patients and providers can do about it.
view more