Multicultural Pharmacy: Bridging Language, Culture, and Medication Safety
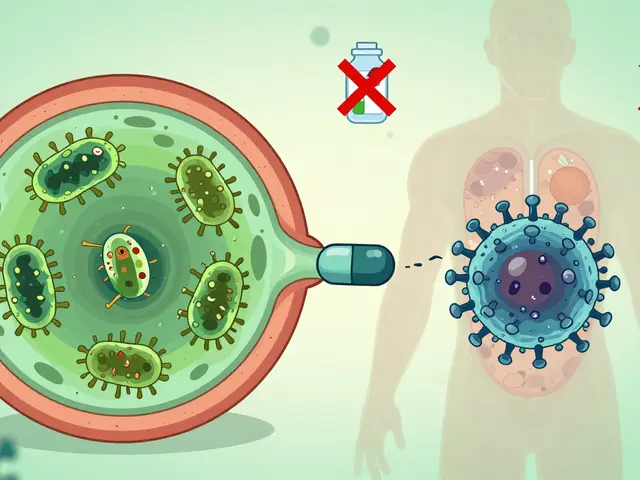
When it comes to taking medication, multicultural pharmacy, the practice of delivering pharmaceutical care that respects cultural, linguistic, and social differences. Also known as culturally competent pharmacy, it’s not just about translating labels—it’s about understanding why someone might skip their pills because they think it’s bad luck, or why they won’t ask questions because their last doctor made them feel stupid. This isn’t theoretical. A study from the CDC found that patients with limited English proficiency are 30% more likely to have a medication error. And it’s not always the language. It’s the belief that herbs are safer than pills, that pain means the medicine is working, or that a doctor’s advice doesn’t apply to their family’s traditions.
Language barriers in pharmacy, the challenge of communicating drug instructions when patients and pharmacists don’t share a common language are one of the biggest problems. A Spanish-speaking patient might be told to take "una pastilla cada día" but misunderstand it as "una pastilla cada vez que duele." That’s not just a mistake—it’s dangerous. And it’s not just Spanish. In Canada, pharmacists serve people who speak over 200 languages. Using Google Translate on a prescription label doesn’t cut it. You need trained interpreters, visual aids, and pharmacists who know how to ask open-ended questions instead of assuming understanding.
Cultural competence, the ability of healthcare providers to deliver care that aligns with a patient’s cultural beliefs, values, and practices isn’t optional. It’s the difference between a patient refilling their blood pressure med or hiding it because they think it makes them "weak." In some cultures, taking daily pills for a silent condition like hypertension feels like admitting you’re sick. In others, mixing traditional remedies with prescription drugs is normal—until it causes liver damage. Multicultural pharmacy means asking, "What are you taking at home?" not "Are you following your prescription?"
Medication adherence, the degree to which patients take their meds as prescribed drops sharply when culture and language aren’t respected. One study showed that African American patients with diabetes were 50% more likely to miss doses if their pharmacist didn’t acknowledge their spiritual beliefs about health. Meanwhile, Southeast Asian elders might avoid insulin because they fear it’s "poison"—a fear rooted in past experiences with unsafe drugs in their home countries. Fixing adherence isn’t about nagging. It’s about listening, adapting, and building trust.
And then there’s health disparities, systematic differences in health outcomes between groups based on race, income, language, or immigration status. These aren’t accidents. They’re built into how care is delivered. A refugee from Syria might not know how to refill a prescription online. A low-income Indigenous patient might skip meds because they can’t afford the co-pay and don’t know about patient assistance programs. Multicultural pharmacy doesn’t ignore these gaps—it fights them. It’s about having bilingual staff, culturally tailored handouts, and pharmacists who walk into a home and don’t judge the herbs on the counter.
What you’ll find in these posts isn’t theory. It’s real-world fixes. From how to spot when a patient is hiding their true medication use, to why a simple pill organizer won’t work for someone who reads right-to-left, these articles show what actually works on the ground. You’ll learn how to ask the right questions, how to spot hidden risks in polypharmacy among elderly immigrants, and why health literacy campaigns fail when they don’t speak the patient’s language—literally and culturally. This isn’t about being politically correct. It’s about saving lives.

Multicultural Perspectives on Generics: How Culture Shapes Patient Trust and Adherence
Cultural beliefs about pill appearance, ingredients like gelatin, and trust in healthcare shape how patients use generic medications. Learn how religion, color, and misinformation affect adherence - and what patients and providers can do about it.
view more