Cultural Competence in Pharmacy: Why It Matters for Medication Safety and Trust
When someone doesn't take their blood pressure pill because they think it's "too Western" or skips insulin because they fear side effects no one explained in their language, that's not just noncompliance—it's a failure of cultural competence, the ability of healthcare providers to understand and respect patients' cultural backgrounds, beliefs, and communication styles to deliver effective care. Also known as cultural humility, it's not optional in pharmacy—it's the difference between a patient getting better and ending up in the hospital.
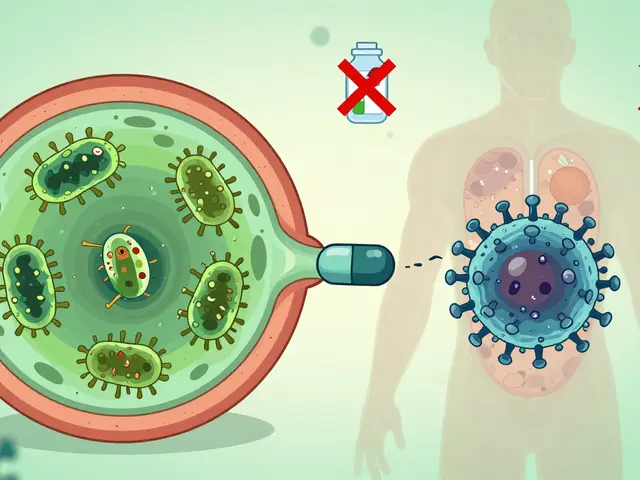
Cultural competence directly affects health literacy, a patient's ability to understand medical information and make informed decisions about their treatment. If a pharmacist assumes everyone knows what a generic drug is—or that everyone trusts the FDA—they're missing the point. Many people, especially older adults or immigrants, don't know generics are chemically identical to brand names. They think they're getting "weaker" medicine. That fear? It’s cultural. It’s rooted in past experiences, misinformation, or language gaps. And it kills. Same with polypharmacy. An elderly patient on ten pills might not say they’re confused—they might nod along because asking questions feels disrespectful in their culture. That’s why checklists like the Beers Criteria only work if the provider asks the right questions in the right way.
Patient trust, the belief that a healthcare provider has the patient’s best interest at heart and will communicate clearly and respectfully doesn’t come from a fancy brochure. It comes from a pharmacist who learns how to say "your medicine" in their native tongue, who asks, "What do you think this pill does?" instead of just reading off instructions. It comes from knowing that some communities avoid certain drugs because of historical harm—like the Tuskegee study or forced sterilizations—and that distrust doesn’t vanish with a prescription. Cultural competence means recognizing that a patient’s religion, diet, family structure, or past trauma can change how they view a pill. A Muslim patient might refuse a capsule with gelatin. A refugee might hide their meds because they fear authorities. A single mom might skip doses because she can’t afford to miss work. These aren’t compliance issues—they’re systemic gaps.
And it’s not just about language. It’s about timing. Some cultures prioritize family decisions over individual choices. Some see illness as spiritual, not chemical. If your pharmacy only hands out printed leaflets in English, you’re not helping—you’re excluding. Real cultural competence means training staff to listen more than they talk, to ask open questions, and to adapt. It means knowing when to bring in a translator who’s trained in medical terms—not just a bilingual cousin. It means understanding that a patient who says "I’m fine" might actually mean "I’m scared and don’t know how to ask for help." This collection of articles doesn’t just talk about drugs—it talks about people. You’ll find guides on how to spot when someone misunderstands their meds because of cultural barriers, how to reduce dangerous interactions by listening first, and how to make lab monitoring calendars work for patients who don’t speak the same language as their doctor. You’ll see how gut bacteria, penicillin allergies, and steroid shots all connect to the same truth: medicine only works when people understand it, trust it, and feel seen while taking it.

Multicultural Perspectives on Generics: How Culture Shapes Patient Trust and Adherence
Cultural beliefs about pill appearance, ingredients like gelatin, and trust in healthcare shape how patients use generic medications. Learn how religion, color, and misinformation affect adherence - and what patients and providers can do about it.
view more