20 Jan |
11:17 AM

Ever lay awake at night wondering why you’re exhausted even after eight hours in bed? You snore loudly. You wake up gasping. Your partner says you stop breathing. Or maybe you just feel like you’re never truly rested - no matter how much you sleep. If this sounds familiar, you might be dealing with a sleep disorder. And the most accurate way to find out what’s going on? A polysomnography - commonly called a sleep study.
What Exactly Is a Polysomnography?
Polysomnography isn’t just a fancy term. It’s the gold standard for diagnosing sleep disorders. The word breaks down simply: poly means many, somno means sleep, and graphy means recording. So, it’s a test that records many things while you sleep. Unlike a quick home test that only checks your breathing, polysomnography watches your whole sleep. It tracks brain waves, eye movements, heart rate, muscle activity, oxygen levels, breathing patterns, and even body position. All of this happens overnight in a sleep lab, under the watch of trained technicians. This level of detail matters because sleep isn’t just resting. It’s a complex cycle of stages - light sleep, deep sleep, and REM sleep - that repeat every 90 minutes. If your body skips stages, wakes up too often, or doesn’t get enough deep or REM sleep, it throws off your whole system. That’s when problems like sleep apnea, narcolepsy, restless legs, or night terrors show up.What Happens During the Test?
You’ll arrive at a sleep center about an hour before your usual bedtime. The room looks like a hotel room - comfortable bed, quiet, temperature kept between 68 and 72°F. No fancy machines. Just sensors. A sleep technologist will attach around 20 small electrodes and sensors to your scalp, face, chest, legs, and fingers. These aren’t needles. They’re sticky patches that pick up signals. One goes on your chin to track muscle movement. Two go near your eyes to catch rapid eye movements. A belt around your chest and belly measures breathing effort. A tiny sensor on your finger checks oxygen levels. And a soft tube under your nose records airflow. You’ll also have a small microphone and camera in the room to record snoring or unusual movements - like kicking, yelling, or getting out of bed. All of this is completely painless. The hardest part? Getting used to the feeling of being wired up. Once you’re settled, the lights go off. The technologist watches your sleep from another room on a screen, monitoring everything in real time. They can talk to you through an intercom if you need to use the bathroom or feel uncomfortable. Most people fall asleep within an hour. Even if you don’t sleep as well as you do at home, it’s usually enough data to make a diagnosis.What Does the Test Measure?
Here’s what polysomnography actually tracks - and why each one matters:- EEG (brain waves): Shows which sleep stage you’re in - NREM (stages 1-3) or REM. This is how doctors spot if you’re skipping deep sleep or jumping straight into REM, which happens in narcolepsy.
- EOG (eye movements): Detects rapid eye movements that mark REM sleep. If you enter REM too quickly or too often, it’s a red flag.
- EMG (muscle activity): Monitors muscle tone. Low tone in REM is normal. High tone in legs? Could mean restless legs syndrome. Sudden jerks? Might be periodic limb movement disorder.
- ECG (heart rhythm): Checks for irregular heartbeats that happen during sleep, like atrial fibrillation, which is common in people with sleep apnea.
- Respiratory effort: Belts around your chest and belly tell if you’re trying to breathe - even if air isn’t getting through.
- Airflow: Sensors near your nose detect if air is moving. No airflow? That’s an apnea.
- Oxygen saturation: A pulse oximeter on your finger shows how much oxygen your blood carries. If it drops below 90%, your brain wakes you up - even if you don’t remember it.
- Body position: Some people only have apneas when lying on their back. This helps doctors recommend positional therapy.
- Audio/video: Records snoring, talking, screaming, or walking in your sleep - signs of parasomnias.
How Are Results Interpreted?
After the night is over, the data is downloaded. A board-certified sleep doctor spends 2 to 3 hours reviewing it. The raw data can be over 1,000 pages long. The key numbers they look at:- AHI (Apnea-Hypopnea Index): How many breathing pauses or shallow breaths you have per hour. Less than 5 is normal. 5-15 is mild sleep apnea. 15-30 is moderate. Over 30 is severe.
- Desaturation events: How often your oxygen drops below 90%. More than 5 per hour is concerning.
- Sleep efficiency: Percentage of time you were actually asleep vs. lying in bed. Below 85% suggests poor sleep quality.
- Time in REM and deep sleep: Healthy adults spend about 20-25% of sleep in REM and 15-20% in deep sleep. Less than that? You’re not recovering properly.
- Leg movements: More than 5 per hour during sleep can point to restless legs or periodic limb movement disorder.

Split-Night Studies: One Night, Two Tests
If your sleep study shows severe sleep apnea early in the night - say, an AHI over 30 - the technician might switch you to a split-night study. That means after the diagnostic portion, they’ll wake you up, fit you with a CPAP mask, and adjust the pressure while you sleep. This saves a second trip. About 35% of sleep studies in the U.S. are now split-night studies. It’s efficient. And it means you can start treatment the same night.Polysomnography vs. Home Sleep Tests
You might have heard about home sleep tests. They’re cheaper, easier, and you sleep in your own bed. But they’re limited. Home tests usually only measure:- Airflow
- Breathing effort
- Oxygen levels
- Heart rate
What If the Results Are Normal?
Sometimes, the test comes back clean. No apnea. No leg movements. No unusual brain patterns. But you still feel tired. That’s when doctors look at other factors: your sleep schedule, stress levels, caffeine intake, or even undiagnosed depression. They might recommend a Multiple Sleep Latency Test (MSLT) - a daytime nap study - to check for narcolepsy or excessive daytime sleepiness. Or they might suggest keeping a sleep diary for a few weeks. Sometimes, the problem isn’t a disorder - it’s poor sleep hygiene. Too much screen time. Irregular bedtimes. Late-night coffee.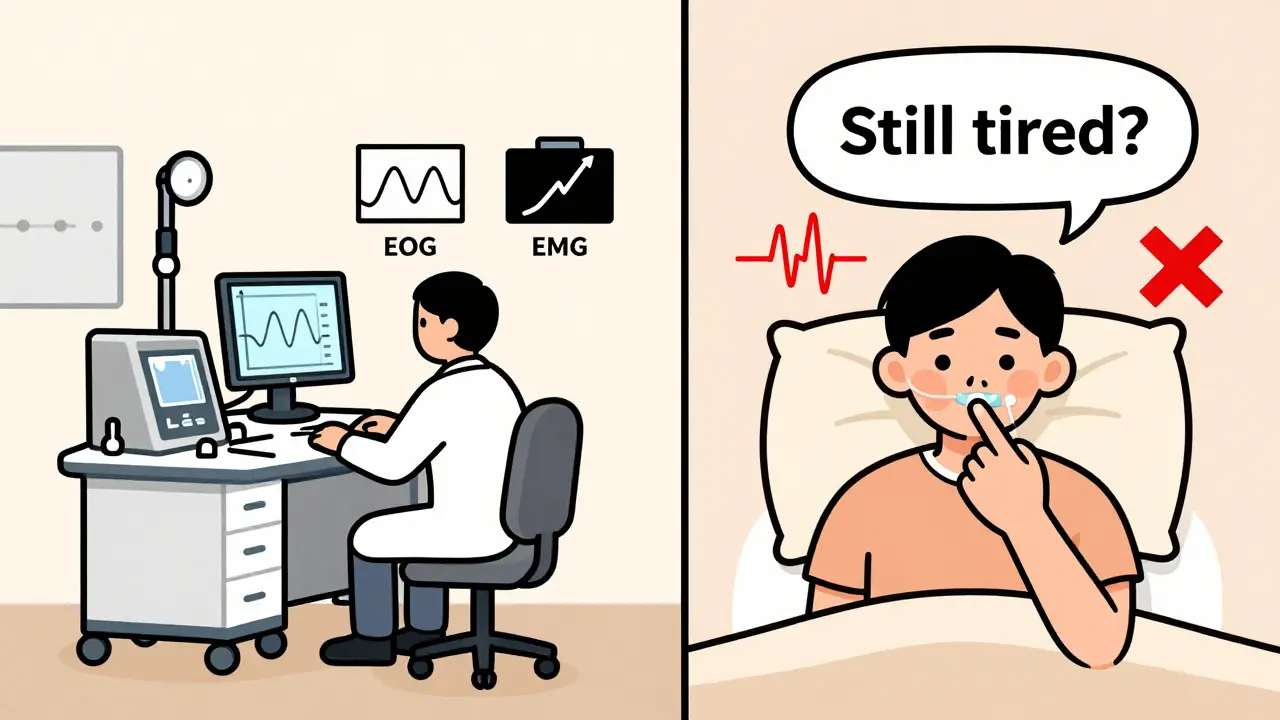
Insurance and Costs
In the U.S., Medicare covers 80% of polysomnography if your symptoms match their criteria - loud snoring, witnessed apneas, daytime sleepiness. Private insurers usually require prior authorization. You’ll need documentation from your doctor showing you’ve tried lifestyle changes first. The cost of an in-lab study ranges from $1,000 to $3,000. Home tests are $200-$500. But if the home test fails or misses something, you’ll end up paying more in the long run.How to Prepare for Your Sleep Study
Don’t treat it like a hospital visit. Treat it like a good night’s sleep - just with extra sensors.- Stick to your normal sleep schedule for 3-4 days before the test.
- Avoid caffeine after noon the day before.
- Don’t nap in the afternoon.
- Wash your hair - no gels, oils, or sprays. The electrodes need to stick to clean skin.
- Bring comfortable pajamas, toiletries, and anything that helps you sleep - a pillow, book, or calming music.
- Let the tech know if you’re anxious. They’ve seen this a thousand times. They’ll help you relax.


9 Comments