
Polypharmacy Risk Checker
Check Your Medications for Dangerous Interactions
Enter your medications to see if you have dangerous combinations. This tool uses the Beers Criteria to identify high-risk medications for older adults.
Results will appear here after checking your medications
Important: This tool is for informational purposes only. Always consult your pharmacist or doctor before making any changes to your medications.
More than 1 in 3 adults over 60 are taking five or more prescription drugs. That’s not just common-it’s a ticking time bomb. Many people don’t realize that taking a blood pressure pill, a sleep aid, and an over-the-counter cold medicine together can send them to the ER. It’s not about taking too many pills-it’s about which ones are being taken together. The right checklist can stop a bad reaction before it starts.
What Exactly Is Polypharmacy?
Polypharmacy means taking five or more medications at the same time. It’s not always wrong. Someone with diabetes, heart disease, high blood pressure, and arthritis might need all those drugs to survive. But the problem isn’t the number-it’s the hidden clashes. Two drugs that are safe alone can turn dangerous when mixed. A 2022 CDC report found that 33% of people in their 60s and 70s are on five or more prescriptions. And for cancer patients? Nearly 6 in 10 start chemotherapy already on five or more meds.Each extra pill adds risk. Research shows every additional medication increases your chance of a serious drug interaction by nearly 40%. That’s not a small jump. It’s a steep climb. And those interactions aren’t theoretical. They land people in hospitals. In the U.S., over 1.3 million emergency visits each year are tied to bad drug combos. Almost 350,000 of those patients end up admitted. Most are older adults. Most were taking meds they thought were harmless.
The Deadliest Combinations You Might Not Know About
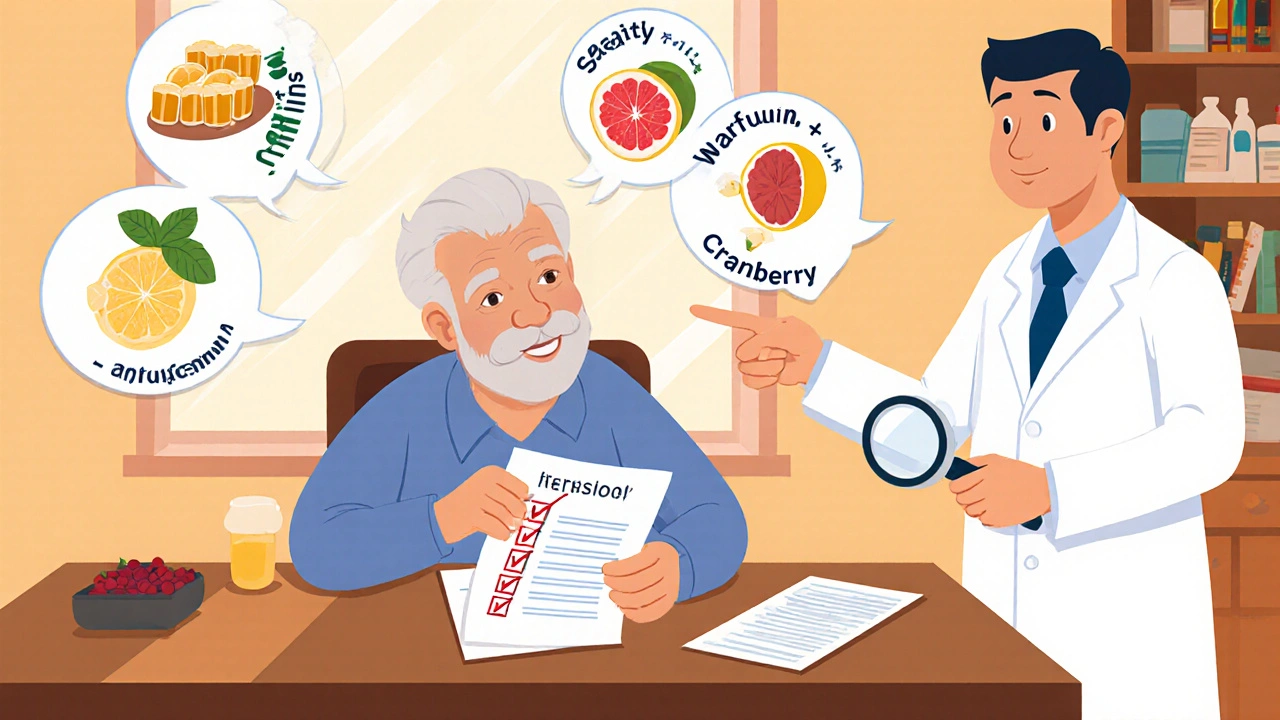
Some drug pairs are like gasoline and a match. They’re quiet until they explode.- Warfarin + cranberry juice: Warfarin thins your blood. Cranberry juice makes it thinner-too thin. Bleeding risk spikes. People think juice is healthy. It’s not when you’re on blood thinners.
- Statins + grapefruit juice: Statins lower cholesterol. Grapefruit blocks how your body breaks them down. Too much statin builds up. Muscle tissue starts dying. That’s rhabdomyolysis-a life-threatening condition.
- Blood pressure meds + decongestants (like pseudoephedrine): Decongestants tighten blood vessels. Blood pressure meds try to relax them. The result? A dangerous spike in pressure. One study found this combo caused hospitalizations in seniors using OTC cold meds.
- Acetaminophen + oxycodone + prochlorperazine: This trio showed up too often in ER visits in the 30 days before admission. Acetaminophen and oxycodone are common painkillers. Prochlorperazine is for nausea. Together, they can cause extreme drowsiness, confusion, and even respiratory depression.
And don’t forget the silent players: supplements. A 2022 study of cancer patients found that 40% of dangerous interactions came from vitamins, herbs, or minerals-not prescriptions. Calcium, magnesium, and even vitamin D can interfere with how your body handles other drugs.
The Beers Criteria: The Gold Standard for Risk
Doctors and pharmacists use a tool called the Beers Criteria to spot risky drugs in older adults. It’s updated every few years, and the 2019 version is still the go-to. It flags medications that are more likely to cause harm than help in people over 65.Here’s what it warns against:
- Anticholinergics: Drugs like diphenhydramine (Benadryl), oxybutynin, and even some antidepressants. These cause brain fog, dry mouth, constipation, and confusion. They’re often prescribed for allergies, bladder issues, or sleep-but the risks outweigh the benefits for seniors.
- Benzodiazepines: Lorazepam, diazepam, alprazolam. These are sedatives. They increase fall risk by 50%. One fall can mean a broken hip, surgery, and never walking the same again.
- Alpha-blockers: Doxazosin, terazosin. Used for high blood pressure or prostate issues. But they drop blood pressure too fast when standing. Dizziness. Falls. ER visits.
The Beers Criteria isn’t a ban list. It’s a red flag. If your doctor prescribes one of these, ask: Is this still necessary? Is there a safer alternative?
Prescribing Cascades: When One Drug Creates Another Problem
Here’s how it often goes: You take a painkiller. It causes constipation. So you get a laxative. The laxative makes you lose potassium. Now you need a potassium supplement. Then you get muscle cramps. So you get a muscle relaxant. Suddenly, you’re on eight meds instead of two.This is called a prescribing cascade. It’s not malpractice. It’s systemic. Often, no single doctor sees the whole picture. Your cardiologist prescribes one thing. Your rheumatologist prescribes another. Your PCP doesn’t know what’s on the list. And you’re left trying to keep track.
A 2020 study of seniors in Ohio found 67% were taking at least one medication that didn’t belong. One woman was on six drugs for sleep, anxiety, and pain. She didn’t realize her confusion and dizziness were from the mix-not aging. She was prescribed a new antidepressant to treat the confusion. That made it worse.
Your Polypharmacy Risk Checklist
This isn’t a doctor’s form. It’s your personal safety tool. Keep it in your wallet. Bring it to every appointment.- List every pill, patch, liquid, and supplement. Include OTC meds (ibuprofen, antacids), vitamins, herbal teas, and CBD oils. Don’t skip anything.
- Check for Beers Criteria drugs. Look up each one. If it’s on the list, ask your pharmacist or doctor why it’s still needed.
- Look for red-flag combos. Use the list above. Do you have warfarin and cranberry juice? Statins and grapefruit? Blood pressure meds and decongestants?
- Ask: What is this for? If you can’t explain why you take a drug, it might not be needed. Many seniors take meds they’ve been on for years without review.
- Check for duplication. Is your blood pressure pill the same as the one in your combo pill? Are you taking Tylenol and Percocet? Both have acetaminophen. Too much can wreck your liver.
- Review food interactions. Grapefruit. Cranberry. Dairy. Alcohol. These aren’t just warnings on labels. They’re real dangers.
- Bring this list to every appointment. Not just your doctor. Your dentist, physical therapist, ER doctor-all need to know what you’re taking.
Use the ARMOR tool: Assess, Review, Minimize, Optimize, Reassess. It’s a simple framework used by pharmacists and cancer centers. One 72-year-old cancer patient cut their meds from 12 to 7 using this method. Their energy improved. Their confusion lifted. They didn’t lose any treatment effectiveness.

Who Should You Talk To?
Your doctor might not know every interaction. Your pharmacist does.Pharmacists are trained to spot drug clashes. They know that taking a statin with a certain antibiotic can cause kidney damage. They know that some antacids block thyroid meds. They’re the unsung heroes of medication safety.
Ask for a medication therapy review. Many pharmacies offer it for free. Bring your full list. Ask: “Which of these can I stop? Which are dangerous together? Which have safer alternatives?”
If you’re on Medicare, you may qualify for a free annual medication review under your Part D plan. Call your plan. Ask for it. Don’t wait for your doctor to bring it up.
What Happens When You Act?
People who use a checklist and get help reducing unnecessary meds don’t just avoid ER visits. They feel better.One study found that after a pharmacist-led review, 62% of seniors reduced their pill count. Of those, 80% reported improved energy, fewer falls, and less confusion. Not because they stopped needed meds-but because they stopped the ones that were hurting them.
It’s not about cutting drugs. It’s about cutting risk. It’s about making sure every pill you take is working for you-not against you.
What’s Next?
The future of polypharmacy safety is coming. Some hospitals now use AI to scan your entire med list and flag dangerous combos in real time. Smart pill bottles track if you’re taking meds correctly. Wearables detect early signs of dizziness or heart rhythm changes.But none of that helps if you don’t start today. You don’t need fancy tech. You need a list. A question. A conversation.
Right now, open your medicine cabinet. Write down every pill, capsule, and bottle. Then call your pharmacist. Say: “I’m on five or more meds. Can you help me check if any of them are dangerous together?”
That one call could save your life.
What is the most common dangerous drug combination in older adults?
The most common dangerous combo involves blood pressure medications paired with over-the-counter decongestants like pseudoephedrine. This combination can cause a sudden, dangerous spike in blood pressure. Other frequent risks include warfarin with cranberry juice and statins with grapefruit juice-all of which are often overlooked because they involve common products.
Can I stop my meds if I feel fine?
Never stop a prescription without talking to your doctor or pharmacist. But if you’re feeling fine, ask: “Is this still necessary?” Many older adults take medications for conditions that have since improved or resolved. A review might show you can safely reduce or stop one or more drugs without harm.
Do supplements count as medications in a polypharmacy risk check?
Yes. Supplements like calcium, magnesium, vitamin K, fish oil, and herbal products like St. John’s Wort can interact with prescription drugs. In fact, nearly 40% of dangerous interactions in older adults involve supplements-not prescriptions. Always list them on your medication checklist.
How often should I review my meds?
Review your full medication list at least once every six months. Also review it after any hospital stay, new diagnosis, or if you start or stop any medication-even if it’s OTC. Changes in health, weight, or kidney function can change how your body handles drugs.
Is polypharmacy always bad?
No. If you have multiple chronic conditions like heart failure, diabetes, and arthritis, you may need several medications to stay healthy. The problem isn’t the number-it’s whether each drug is necessary, effective, and safe with the others. The goal isn’t to take fewer pills-it’s to take the right ones.
Can my pharmacist help me reduce my meds?
Yes. Pharmacists are trained to identify unnecessary, duplicate, or dangerous medications. Many offer free medication reviews. They can work with your doctor to create a safe tapering plan for drugs that can be reduced or stopped. Don’t wait for your doctor to bring it up-ask your pharmacist first.
Still unsure? Keep your checklist. Bring it to your next appointment. Ask one question: “Could any of these meds be hurting me more than helping?” That’s the first step to safer, simpler, and healthier living.


18 Comments
This post hit me right in the gut-my mom’s on eight meds and she swears she’s fine, but she’s been stumbling around like a drunk toddler since last winter. I didn’t realize half of it was unnecessary until I printed this checklist and took it to her pharmacist. She cried. Not from sadness-from relief. We cut three drugs. She sleeps better. She remembers my name again. This isn’t just medical advice-it’s a lifeline.
People like you think supplements are harmless. Wrong. My aunt took fish oil with warfarin. Blew a vessel in her brain. Dead in 48 hours. You’re lucky you didn’t kill someone.
Love this. I’m a caregiver for my dad and I’ve been keeping a running list since last year. I started with a notebook, now it’s a Google Doc shared with his whole care team. Even his dentist asked for it. One time, they caught him on two different versions of the same blood pressure med. Saved his kidneys. Small wins matter.
Bro. I just Googled ‘grapefruit + statins’ after reading this and my heart stopped. My pops takes Lipitor and drinks grapefruit juice every morning like it’s a spiritual ritual. I’m taking his juice away today. No mercy. He’ll hate me. But he’ll live. 💪
My grandma was on Benadryl for sleep for 12 years. No one ever questioned it. She got diagnosed with early dementia at 78. The doctor said it was likely the anticholinergics. We weaned her off slowly. Within three months, she started recognizing my kids again. I wish I’d known this sooner.
OMG I just checked my meds and I’m on three things from the Beers list. I’m 52. Am I already old? Do I need to start writing my will? 😭
From a clinical pharmacy standpoint, the prescribing cascade phenomenon is under-recognized in primary care settings. The absence of centralized medication reconciliation protocols leads to iatrogenic polypharmacy, particularly in geriatric cohorts with multimorbidity. The ARMOR framework is evidence-based and aligns with the 2023 Beers Criteria update-particularly in deprescribing anticholinergics and benzodiazepines.
I’ve been meaning to do this for my dad but I’m scared to ask. What if he thinks I’m trying to take away his independence? What if he gets mad? I just want him to be safe…
In India, we don’t have pharmacists doing reviews. We have aunties who sell pills from their kitchen counters. My uncle took 12 different painkillers because the shopkeeper said ‘mix them, better effect’. He ended up in ICU with liver failure. This checklist should be printed on every medicine bottle. Everywhere.
While I appreciate the intent of this article, the empirical validity of the Beers Criteria is increasingly contested in light of recent longitudinal cohort studies (see JAMA Internal Medicine, 2023). The framework was developed for institutionalized elderly populations and may not generalize to ambulatory, high-functioning seniors. Additionally, the exclusion of pharmacogenomic factors (e.g., CYP450 polymorphisms) renders many interaction warnings statistically non-specific. A more nuanced, biomarker-informed approach is warranted.
Most people don’t realize that calcium supplements interfere with levothyroxine absorption. My mom was on both. Her TSH kept creeping up. Turns out she was taking calcium at breakfast, and levothyroxine at bedtime. Simple fix: space them 4 hours apart. No new meds. No drama. Just timing.
And yet, somehow, we still let doctors prescribe Ambien to 80-year-olds. What’s next? Prescribing Xanax to toddlers? This isn’t medicine-it’s a pharmaceutical carnival. Someone’s making money off this. Someone’s profiting off confusion. Wake up.
I’m from India and I’ve seen this firsthand. My uncle took 14 pills a day. We got him to a pharmacist. Cut it to 5. He started walking again. He started laughing again. I’m not saying all meds are bad. I’m saying: ask. Always ask. Don’t let fear keep you silent. Your life is worth it.
So let me get this straight… you want us to trust a pharmacist more than our doctor? 😏 I mean… sure, if your doctor is a 70-year-old who thinks ‘digital’ means a type of watch.
It’s not about the number of pills. It’s about the silence around them. We don’t talk about meds like we talk about food or exercise. We just swallow them. Like prayers. Like curses. Maybe the real problem isn’t the drugs-it’s that we’ve stopped asking why we’re taking them.
Look, I get it. You’re scared of pills. You think every drug is a poison. But let’s be real-most of these people are on meds because they’re dying. Cancer. Heart failure. Stroke. You think stopping a beta-blocker because someone drank grapefruit juice is going to save them? No. It’s going to kill them faster. This checklist is great for the healthy elderly. For the sick? It’s dangerous nonsense. You’re playing doctor with lives. Stop.
As an American citizen who has served his country with honor and maintains a strict adherence to constitutional principles, I must emphasize that this article is a clear example of the creeping overreach of the pharmaceutical-industrial complex. The Beers Criteria, developed by unelected medical bureaucrats, undermines personal liberty and the sacred right to self-medicate. We must resist this tyranny. I have not taken a single pill in 15 years. I am 82. I run marathons. I eat raw garlic. I am proof that nature, not Big Pharma, is the true healer.
Shivam, you’re right to be angry-but don’t let it blind you. My uncle died from a heart attack because he stopped his statin after reading some Reddit post that said ‘statins cause cancer.’ He didn’t know grapefruit made it worse. He didn’t know the real danger was the combo. We need to talk, not just scream.