
What’s Really Happening in Hospitals and Clinics Right Now?
It’s not just about long wait times or packed emergency rooms. The real crisis is deeper: hospitals and clinics across the U.S. are running on empty. Nurses are working double shifts. Doctors are seeing 50% more patients than they should. And in rural areas, some clinics have closed entire units because there’s no one left to staff them.
This isn’t a temporary glitch. It’s the result of years of underinvestment, burnout, and demographic shifts hitting all at once. The healthcare shortages aren’t just about too few people - they’re about too few people doing too much, with too little support.
The Numbers Don’t Lie: Nurses Are Disappearing
In 2025, the U.S. is short more than 78,000 full-time nurses. By 2030, that number could climb past 60,000. And it’s not just nurses. Primary care doctors, mental health counselors, and even medical assistants are in short supply. The American Hospital Association found that 42 states will face serious nursing shortages by 2030.
Why? Half of all nurses are over 50. One in three will retire in the next 10 to 15 years. Meanwhile, nursing schools can’t keep up - they turned away over 2,300 qualified applicants in 2023 because they didn’t have enough faculty to teach them.
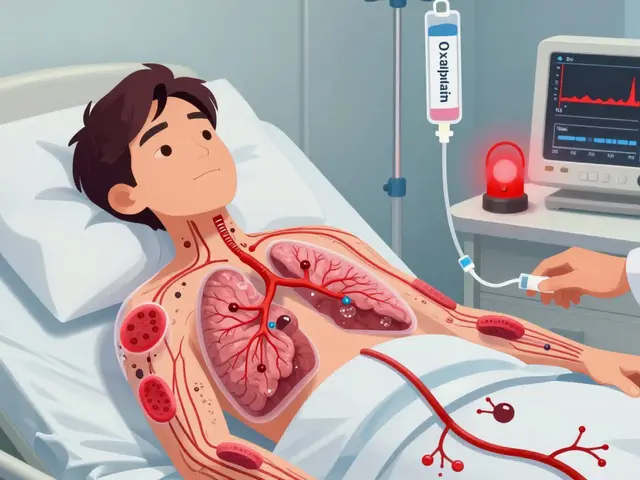
What Happens When There’s No One to Care for You
When hospitals are understaffed, patients pay the price. Studies show that when a nurse is responsible for more than four patients at a time, mortality rates jump by 7%. Emergency rooms see wait times stretch 22% longer. In some rural ERs, patients are waiting 72 hours just to be seen.
It’s not just about delays. Medication errors rise. Infections spread more easily. One ICU nurse in Texas told a Reddit thread she made two near-miss medication mistakes last month because she was managing three critically ill patients alone - a ratio that should never happen.
And it’s getting worse. Hospitals are now using mandatory overtime twice a week just to stay open. Some have created "code lavender" teams - mental health responders for staff who are emotionally broken.
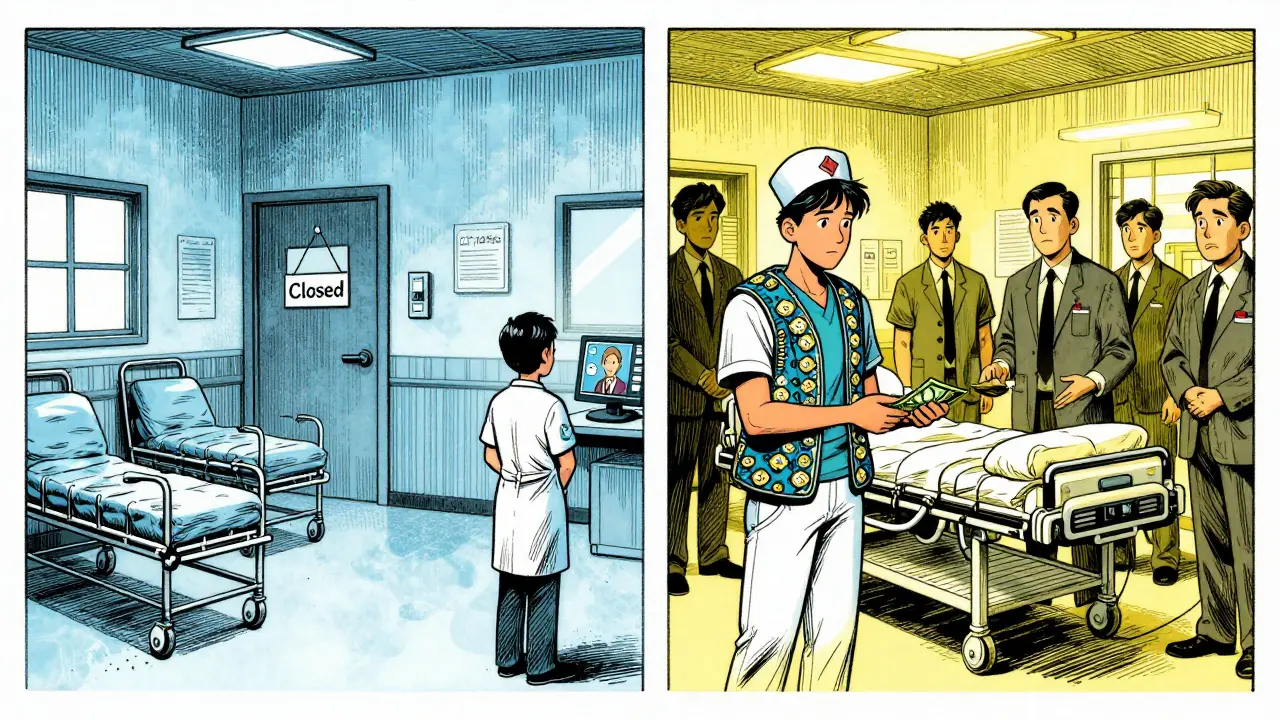
Rural vs. Urban: A Divide That’s Getting Wider
The shortage isn’t spread evenly. Rural hospitals are 37% more likely to have open positions than urban ones. While big city hospitals might be at 82% staffing, rural clinics are hovering around 58%. That means in places like rural Nevada or eastern Kentucky, clinics have shut down outpatient services, stopped accepting new patients, or moved to telehealth-only models - even when patients don’t have reliable internet.
Urban clinics aren’t safe either. But they have more options: they can pay travel nurses $185 an hour to fill gaps. That’s more than double what permanent staff make. It creates tension. It creates resentment. And it doesn’t fix the root problem - it just moves the pain around.
Why the Crisis Keeps Getting Worse
There are three big reasons this isn’t getting better:
- People are leaving. Sixty-three percent of nurses say they’re thinking about quitting. Over 40% say unsafe patient ratios are the main reason.
- Training isn’t keeping up. Federal funding for nursing education is $247 million a year. Experts say it needs to be $1.2 billion. That gap means fewer graduates, fewer teachers, and fewer future nurses.
- The population is aging. There were 55.8 million Americans over 65 in 2023. By 2050, that number will hit 82 million. But the number of working-age people to support them is falling - from four workers per senior today to 2.9 by 2030.
Are Tech Solutions the Answer?
Hospitals are trying AI, telehealth, and automated scheduling tools to fill the gaps. Some are seeing results: telehealth triage cut ER visits by 19% in pilot programs. AI tools can now help with documentation, reducing charting time by up to 30%.
But these aren’t magic fixes. It takes 8.7 weeks to train staff on new tech. EHR systems still don’t talk to each other in 68% of hospitals. And licensing rules block nurses from working across state lines - delays can take over 100 days.
Dr. Robert Wachter from UCSF says technology could cover 30-40% of the gap - but only if hospitals invest seriously. Right now, most are just dipping their toes in.
What’s Being Done - and Why It’s Not Enough
The Biden administration gave $500 million in April 2025 to expand nursing education. That sounds like a lot - until you realize it covers only 18% of what’s needed. The American Hospital Association launched a new program to train 50,000 new workers by 2027. That’s good - but they’re still 500,000 short of what the Health Resources and Services Administration says we’ll need by 2030.
Some states are stepping up. California now requires a 1:5 nurse-to-patient ratio in medical-surgical units. Massachusetts cut its shortage to 8% below the national average with loan forgiveness programs. But most states are still waiting for federal action.

What This Means for You
If you’re a patient, you’re already feeling this. Longer waits. Less time with your doctor. Fewer specialists available. If you need mental health care, you might wait months for an appointment - if you can find one at all. If you’re elderly or have a chronic illness, your care is more fragmented than ever.
If you’re a healthcare worker, you’re exhausted. You’re angry. You’re wondering if you made the right choice. And if you’re a family member watching someone struggle to get care, you’re powerless.
There’s No Quick Fix - But There Is a Path Forward
Fixing this won’t happen with one law or one grant. It needs real, sustained investment:
- Double or triple funding for nursing schools - not just for students, but for teachers.
- Remove state licensing barriers so nurses can move where they’re needed most.
- Pay frontline workers fairly - stop relying on expensive travel nurses as a crutch.
- Let AI help, but don’t let it replace human judgment.
- Make healthcare jobs sustainable - not just profitable.
The Mayo Clinic spent 18 months and $4.7 million redesigning its care teams. Result? Nurse turnover dropped 31%. That’s proof it’s possible - if you’re willing to do the hard work.
Right now, the system is holding together by sheer will. But willpower doesn’t pay bills. It doesn’t prevent infections. It doesn’t bring back nurses who quit. The question isn’t whether we can afford to fix this. It’s whether we can afford not to.
Why are hospitals so short on nurses right now?
Hospitals are short on nurses because half of all nurses are over 50 and nearing retirement, training programs can’t keep up with demand, and burnout from pandemic-era workloads has driven many out of the field. In 2023, nursing schools turned away over 2,300 qualified applicants due to lack of faculty - a 14% increase from the year before.
How do staffing shortages affect patient safety?
When nurses are assigned more than four patients at a time, mortality rates rise by 7%. Medication errors increase, infections spread more easily, and emergency departments see 22% longer wait times. In understaffed units, staff are forced to make split-second decisions with incomplete information - increasing the risk of preventable harm.
Are travel nurses helping or hurting the system?
Travel nurses fill urgent gaps - they made up 12% of hospital staffing in 2023. But they cost 34% more than permanent staff, driving up hospital expenses. Their temporary presence also creates resentment among full-time staff who earn less and work longer hours. While they help avoid shutdowns, they don’t solve the underlying shortage.
Why are rural clinics hit harder than urban ones?
Rural clinics face 37% higher vacancy rates than urban ones because they can’t compete with higher salaries in cities. They also struggle to attract new graduates, lack infrastructure for telehealth, and have fewer training programs nearby. Many have closed entire units or stopped accepting new patients altogether.
Can AI and technology fix the staffing crisis?
AI can help reduce administrative tasks - like documentation - freeing up 30% of a nurse’s time. Telehealth triage has cut ER visits by 19% in some pilot programs. But these tools require training, money, and stable tech systems. In 68% of hospitals, electronic health records still don’t communicate with each other, making tech adoption difficult. Technology can ease the burden, but it can’t replace human care.
What’s the long-term outlook for healthcare staffing?
Without major intervention, nursing shortages could last until 2035. The global healthcare worker gap is expected to peak at 15 million by 2027. Experts say only a combination of better pay, expanded training, policy reform, and technology integration can reverse the trend - and even then, it will take a decade to fully recover.
What Comes Next?
If you’re a patient, document your experiences. Speak up when wait times are dangerous or care feels rushed. If you’re a student considering healthcare, know this: the field is broken - but it needs you more than ever. If you’re a policymaker, stop treating this like a staffing issue. It’s a public health emergency.
The system is still standing. But it’s leaning. And if we don’t shore it up soon, it won’t just be hospitals that fall - it’ll be the trust people have in the care they’re supposed to receive.


13 Comments
The system isn't broken because of lack of will-it's broken because we treat healthcare like a commodity, not a human right. We pay nurses pennies while pharmaceutical CEOs buy private islands. We celebrate innovation in diagnostics but starve the people who actually hold the patient's hand. This isn't about staffing numbers-it's about moral bankruptcy dressed up as policy.
Current staffing models are predicated on a 1990s labor paradigm that no longer aligns with patient acuity or regulatory burden. The nurse-to-patient ratio is a lagging indicator; what we need is real-time workload optimization using predictive analytics integrated with EHR data streams. Until we decouple reimbursement from volume and incentivize outcome-based staffing, we're just rearranging deck chairs on the Titanic.
So let me get this straight-we’re paying travel nurses $185/hour to fix a problem caused by paying permanent staff $35/hour? Brilliant. Just like how we fix a leaking roof by hiring a guy with a bigger bucket. Meanwhile, the nurses who stayed are working 80-hour weeks and being told to ‘practice self-care’ while their hospital’s CEO gets a $12M bonus.
I understand the emotional weight of this issue, but I must emphasize that the root cause is not economic-it is spiritual. The modern healthcare worker has lost their sense of vocation. They no longer see themselves as healers, but as cogs in a machine. Until we restore dignity to the act of caregiving, no policy, no funding, no AI will matter.
You people are delusional. This isn't a shortage-it's a purge. The elite want fewer people alive so they can control the healthcare narrative. Why do you think they shut down rural clinics? To eliminate the ‘unprofitable’ demographic. The fact that you’re surprised by this proves you’ve been brainwashed by the system. Wake up. The nurses aren’t quitting-they’re being pushed out. And the AI? It’s not helping. It’s surveilling. They’re tracking your every keystroke, every shift, every sigh. You think this is about staffing? No. It’s about control.
In my village in Ghana, we don’t have nurses or AI. We have neighbors. We have elders who remember your grandmother’s medicine. We have people who show up with soup when you’re sick. Maybe the answer isn’t more money or tech-it’s rebuilding community. We’ve outsourced care to institutions because we forgot how to care for each other. The real crisis isn’t staffing-it’s loneliness.
Look, I’m not a doctor, but I work in a clinic. Nurses are overworked because hospitals are run like startups trying to maximize profit, not save lives. They hire fewer staff, then blame the nurses when things go wrong. Pay them more. Hire more. Stop pretending this is a ‘system problem.’ It’s a choice.
If people didn’t eat so much junk and get fat, we wouldn’t need so many nurses. This crisis is a direct result of personal irresponsibility. No one forces you to be diabetic. No one forces you to skip your meds. Stop expecting the system to fix your bad choices.
I’ve been a nurse for 22 years. I’ve seen this coming. The system didn’t collapse overnight-it was slowly dismantled by budget cuts, corporate takeovers, and the lie that ‘efficiency’ means less people. I stayed because I love my patients. But I’m not angry anymore. I’m just tired. And I’m not the only one. We need to stop asking nurses to be heroes. We need to stop treating them like disposable labor.
They want to replace American nurses with H-1B visa drones from India and the Philippines. That’s why they’re cutting training programs-so they can import cheap labor. We’re being colonized by healthcare outsourcing. And don’t tell me it’s ‘globalization’-it’s betrayal. We built this system with sweat and sacrifice. Now they want to outsource our dignity too.