Heat Sensitivity
When dealing with heat sensitivity a reduced tolerance to high temperatures that can cause discomfort, dizziness, or heat‑related illness. Also known as temperature intolerance, it often stems from medication side effects, chronic conditions, or lifestyle habits. Imagine stepping outside on a scorching day and feeling light‑headed within minutes—that's heat sensitivity in action. It isn’t just about feeling hot; it’s a signal that your body’s cooling systems are struggling. Recognizing the early signs—excessive sweating, rapid heartbeat, or sudden fatigue—lets you act before a full‑blown heat illness develops. This page pulls together the key factors that make heat sensitivity worse and shows how you can protect yourself when the temperature climbs.
Why Some Medications Heighten Heat Risks
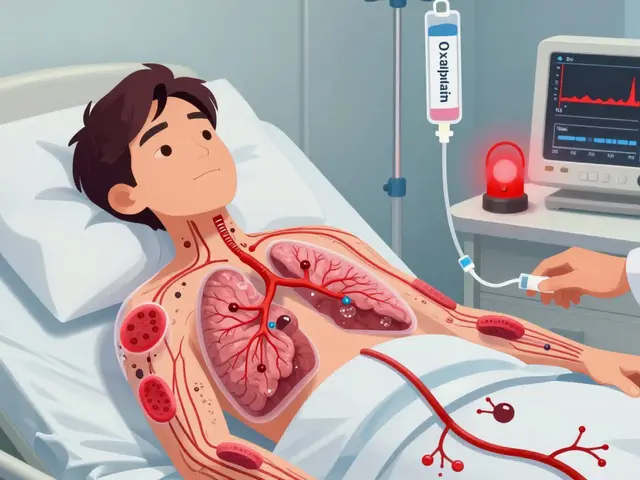
One of the strongest triggers is the use of diuretics drugs that increase urine output and can lower blood volume. When you lose fluid faster than you replace it, your body’s ability to sweat and release heat drops sharply, paving the way for dehydration. Another common culprit is anticholinergic drugs medications that block the neurotransmitter acetylcholine, reducing sweat gland activity. Without enough sweat, the skin can’t evaporate heat, so core temperature spikes quickly. These two drug classes illustrate a clear semantic triple: heat sensitivity is aggravated by diuretics and anticholinergic drugs. The chain continues—lower fluid levels and impaired sweating raise the likelihood of heat illness conditions such as heat exhaustion or heat stroke, especially during prolonged outdoor activity. Understanding this cause‑effect relationship helps you ask the right questions at the pharmacy or doctor’s office.
Beyond meds, everyday habits play a big role. Skipping water, wearing heavy clothing, or exercising during peak sun hours all feed into the same loop: reduced fluid reserves, limited evaporative cooling, and higher core temperature. That’s why dehydration the loss of more fluid than you take in, is both a symptom and a driver of heat sensitivity. When dehydration sets in, blood thickens, the heart works harder, and the brain receives less oxygen, which can trigger dizziness or fainting. This creates another semantic triple: dehydration exacerbates heat sensitivity, which in turn increases the risk of heat illness. By breaking the cycle—hydrating regularly, choosing breathable fabrics, and timing activities for cooler parts of the day—you directly lower the odds of a dangerous heat event.
What should you do if you’re already on a diuretic or an anticholinergic? First, talk to your prescriber about adjusting the dose or switching to a less heat‑sensitive alternative during summer months. Second, adopt a proactive hydration plan: aim for at least 2‑3 liters of water daily, and add electrolytes if you’re sweating heavily. Third, keep a cooling kit handy—wet bandana, portable fan, and a shaded spot can all drop skin temperature within minutes. Finally, monitor your body: a quick check of pulse, skin moisture, and mental clarity tells you whether you’re coping or need to rest. These practical steps turn the abstract risk of heat sensitivity into manageable, everyday actions.
Below you’ll find a curated set of articles that dive deeper into each of these topics. From detailed heat‑precaution guides for diuretic users to broader advice on staying safe in hot weather, the collection equips you with the knowledge to beat heat sensitivity before it beats you.

Procyclidine and Heat Sensitivity: Essential Facts & Management Tips
Discover why procyclidine can cause heat sensitivity, who’s most at risk, and practical steps to stay safe during warm weather.
view more