
Managing multiple medications can feel overwhelming. You’ve got pills for your blood pressure, your diabetes, your cholesterol, maybe some pain relief, vitamins, and herbal supplements. Some you take in the morning, others at night. Some you take with food, others on an empty stomach. And if you miss one, you’re not sure what to do. You’re not alone. Nearly half of people taking chronic medications don’t take them as prescribed. But there’s a simple, powerful tool that changes everything: a medication action plan.
What Is a Medication Action Plan?
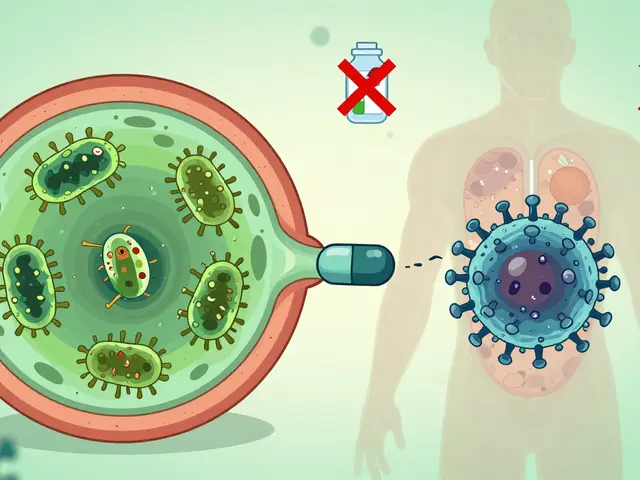
A medication action plan (MAP) isn’t just a list of your drugs. It’s a personalized roadmap created with your care team - your doctor, pharmacist, or nurse - that tells you exactly what to do, when to do it, and what to watch for. Think of it like a GPS for your meds. Instead of guessing, you’ve got clear directions built around your life. It’s not a one-size-fits-all template. A good MAP includes your specific goals, your daily routine, and solutions to the real problems you face - like forgetting pills, side effects, or confusion over doses. It’s written in plain language, not medical jargon. And it’s meant to be updated, not tossed in a drawer after one visit. In the UK and across Europe, these plans are becoming standard. In Germany, since 2016, anyone taking three or more prescribed medicines is legally entitled to a paper-based medication plan updated by their pharmacist each time they pick up a prescription. In the US, Medicare Part D has required Medication Therapy Management (MTM) services - which include MAPs - since 2006. And it works: patients who use a personalized MAP see 25-40% better adherence and up to 32% fewer hospital visits.Why Your Care Team Is Essential
You can’t build a good medication action plan alone. That’s why your care team matters. Your doctor knows your diagnosis. Your pharmacist knows your meds - including what’s over the counter, what interacts with what, and whether you’re taking duplicates. Together, they spot gaps you might miss. For example, you might think your ibuprofen is harmless. But if you’re on blood pressure meds, it can raise your numbers. Or maybe you’re taking two different pills for the same condition - a common mistake when seeing multiple specialists. Your pharmacist can catch that. Your nurse can help you figure out how to fit your doses around your work schedule or bedtime routine. And it’s not just about safety. It’s about empowerment. When you understand why you’re taking each pill - not just that you’re told to - you’re more likely to stick with it. Studies show patients who co-create their MAPs feel more in control. One 68-year-old woman in Birmingham improved her diabetes adherence from 65% to 95% by turning her MAP into a visual chart: coffee cup for morning pills, dinner plate for evening ones.How to Start Building Your Plan
You don’t need to wait for your doctor to bring it up. Take the first step yourself. Here’s how:- Collect everything. Gather every pill, capsule, liquid, patch, or supplement you take - even the ones you only use occasionally. Include vitamins, herbal teas, CBD oils, and over-the-counter painkillers. Don’t leave anything out. Many people forget aspirin or antacids, but these can interact dangerously with prescription drugs.
- Write down your routine. Note when you take each med. Do you take your blood pressure pill with breakfast? Does your cholesterol med go with dinner? Are there days you skip it? Be honest. This isn’t for judgment - it’s for fixing.
- Ask your pharmacist for a review. Most community pharmacies offer free Medication Therapy Reviews. No appointment needed in many cases. Bring your full list. Ask: “Are any of these unnecessary? Do any interact? Is there a simpler way to take them?”
- Schedule a care team meeting. Request a 30-minute appointment with your GP or practice nurse. Say: “I want to make a clear plan for my medications. Can we sit down and build one together?”
What Should Be in Your Plan?
A strong medication action plan includes five key parts:- A complete list of all meds. Name, dose, frequency, purpose (e.g., “Lisinopril 10mg once daily - for high blood pressure”).
- Clear instructions. “Take with food,” “Avoid alcohol,” “Check your pulse before taking.” No vague terms like “as needed.”
- Specific actions. Instead of “take your pills,” say: “Place your morning pills in the small blue box next to your toothbrush.” Or: “Set a phone alarm for 7pm labeled ‘Heart Pill.’”
- Measurable goals. “I will take all my evening meds correctly for 28 days.” Or: “I will call the pharmacy if I feel dizzy more than twice a week.”
- Emergency steps. What to do if you miss a dose? If you feel unwell? Who to call? Include phone numbers - your pharmacist, your GP, and a trusted family member.

Make It Work for Your Life
A plan that doesn’t fit your life won’t be used. That’s why personalization is everything. If you’re blind, ask for a Braille version or audio recording. If you’re hard of hearing, request printed visuals. If you work nights, schedule your doses around your sleep cycle. If you travel often, ask for a travel-sized version with refill reminders. One man in Leeds used sticky notes on his fridge: “Take insulin - after toast.” Another used a pill organizer with different colored compartments labeled “AM,” “PM,” and “As Needed.” He added a small note: “If I feel shaky, eat a biscuit - then call the nurse.” The best plans don’t look like medical documents. They look like your life.What to Do If You’re Not Getting One
If your GP or pharmacist hasn’t offered you a MAP, don’t wait. Ask directly. You’re entitled to one if you take multiple long-term medications. In England, NHS pharmacies can provide medication reviews under the Pharmacy First scheme - no referral needed. Just walk in. In Scotland and Wales, similar services exist. Even if you’re not on Medicare or don’t qualify for public programs, many private insurers now cover MTM services. Call your insurer and ask: “Do you offer Medication Therapy Management? Can I get a personalized action plan?” If you’re told, “We don’t do that here,” ask to speak to the pharmacist. Pharmacists are trained in medication management and often have more time than doctors to sit down and help.Keep It Alive
Your MAP isn’t a one-time thing. It’s a living document. Update it every time:- You start or stop a medicine
- You change doses
- You have a new diagnosis
- You have a hospital stay
- You notice side effects

Real Results, Real People
A 72-year-old woman in Coventry was taking 11 different meds. She didn’t know why she took half of them. After a 45-minute session with her pharmacist, her MAP was cut to 6 essential pills. Two were stopped - they weren’t helping. One was replaced with a once-daily version. She got a visual chart. Within two months, her blood pressure dropped to normal. She stopped falling. She said: “I finally feel like I’m in charge.” Another man in Manchester had been hospitalized three times in a year for low blood sugar. His MAP revealed he was taking his insulin before breakfast - but often skipped breakfast because he worked early shifts. His plan changed: he started taking insulin after eating, and his pharmacist set up automated text reminders. He hasn’t been back to hospital since. These aren’t miracles. They’re results of a simple tool used well.Common Mistakes to Avoid
Don’t fall into these traps:- Using a generic template. Pre-printed plans with no personalization don’t work. If it doesn’t mention your routine, your worries, or your goals - it’s useless.
- Letting someone else write it for you. If your daughter makes the plan but you don’t understand it, you won’t follow it.
- Ignoring over-the-counter meds. Painkillers, antacids, and supplements can cause dangerous interactions.
- Not updating it. A plan from last year is outdated if you’ve changed meds.
- Keeping it hidden. If you’re in an accident and unconscious, no one will know what you’re taking. Keep a copy in your wallet or phone.
Next Steps: What to Do Today
You don’t need to wait for a perfect moment. Start now.- Today: Gather every medication you take - even the ones in the back of your cupboard.
- This week: Book a free Medication Review at your local pharmacy. No appointment? Just walk in.
- Next month: Ask your GP: “Can we build a medication action plan together?”
- Always: Keep your plan visible, update it often, and never be afraid to ask: “Why am I taking this?”
What’s the difference between a medication list and a medication action plan?
A medication list just shows what drugs you take - names, doses, times. A medication action plan goes further. It tells you what to do, why it matters, and how to handle problems. It includes personal goals, step-by-step actions (like “put pills by your toothbrush”), and emergency instructions. It’s not just information - it’s a guide to living well with your meds.
Can I make a medication action plan myself without a care team?
You can write a draft, but you shouldn’t rely on it alone. Without a pharmacist or doctor, you might miss dangerous interactions, unnecessary duplicates, or outdated prescriptions. A care team brings expertise you can’t get from an app or a website. They can tell you what to stop, what to change, and what’s safe. Always get their input before finalizing your plan.
Do I need a medication action plan if I only take one or two medicines?
If you’re taking just one or two meds and they’re simple - like a daily blood pressure pill and a vitamin - you might not need a formal plan. But if you’re ever confused about when or why to take them, or if you’ve missed doses before, a plan helps. Even simple regimens benefit from clear goals and reminders. It’s not about quantity - it’s about confidence.
Are medication action plans covered by the NHS?
Yes, in many cases. Under the NHS Pharmacy First scheme, you can get a free Medication Review at any community pharmacy - no GP referral needed. If you take multiple long-term medicines, you’re eligible. Some areas also offer Medication Therapy Management through GP practices. Ask your pharmacist or call NHS 111 to find out what’s available near you.
What if my care team won’t help me make a plan?
If your GP or pharmacist says no, ask why. Sometimes it’s just a matter of not knowing the service exists. Say: “I’ve heard about medication action plans - can you help me get one?” If they still refuse, go to another pharmacy. Most community pharmacists are trained to do this. You can also contact your local Patient Advice and Liaison Service (PALS) for support. You have the right to clear, personalized information about your medications.
How often should I update my medication action plan?
Update it every time your meds change - whether you start, stop, or change a dose. Also update it after a hospital visit, a new diagnosis, or if you notice side effects. Even if nothing changes, review it every six months. Your life changes - your plan should too. A plan that hasn’t been updated in a year is likely out of date.
Can I use a smartphone app for my medication action plan?
Yes - but only as a tool, not a replacement. Apps can send reminders, track doses, and store your list. But they don’t replace the personalized advice from your care team. The best approach: use an app to remind you, but keep a printed or digital version of your official MAP created with your pharmacist or doctor. That’s the document you bring to appointments and emergencies.


13 Comments
People don't need a plan. They need to stop being lazy. If you can't remember to take your pills, maybe you shouldn't be taking them. I've been on 8 meds for 12 years and I just use a pillbox. No therapist, no pamphlet, no 'action plan.' Just discipline. Stop making everything so complicated.
Let’s be real - this whole MAP thing is just bureaucratic theater. The US spends billions on ‘medication adherence programs’ while ignoring the root problem: pharmaceutical companies price gouge so hard people can’t afford their meds. You give someone a fancy color-coded chart and then charge them $400 for insulin. That’s not empowerment. That’s cruelty dressed up as care.
Just had my med review at the pharmacy yesterday and it was eye-opening. Turns out I was taking two different versions of the same BP med - one from my doc, one from a telehealth visit. The pharmacist caught it immediately. Also found out my ginkgo biloba was messing with my blood thinner. They printed me a simple one-page plan with emojis for times of day. I put it on my fridge. Game changer.
The concept of a medication action plan is not merely a logistical tool but a profound epistemological shift in the patient-provider relationship. It transforms the patient from a passive recipient of pharmaceutical directives into an active co-architect of their own physiological equilibrium. This is not a document - it is a covenant of trust, a dialectical space where medical authority and lived experience converge to produce a form of therapeutic agency previously unattainable in the fragmented, siloed structures of modern healthcare. The cultural and systemic implications of this shift, particularly in non-Western contexts where familial caregiving often supersedes institutional support, warrant further sociological inquiry.
I love this so much. My mom is 81 and was mixing up her meds until we made a visual chart with pictures. She points to the banana for her potassium pill, the sun for morning meds, the moon for night. She says it feels like she’s playing a game now instead of being punished by her own body. I printed it laminated. She keeps it by her coffee maker. We should all do this. It’s not rocket science, it’s love.
Man, I used to think meds were just pills you swallow and forget. Then my uncle got hospitalized because he was taking aspirin with his blood thinner and no one told him it was a bad combo. After that, we made a MAP together - handwritten on a big poster board with sticky notes for refills. Now he’s got his own ‘Medication Wall’ in his living room. It’s like a shrine to survival. I’m telling everyone I know. This isn’t healthcare. This is heroism.
Wow 🙌 This is exactly what my grandma needed! She was taking 14 meds and couldn’t remember half of them. We sat down with her pharmacist and made a simple plan with color-coded pill boxes and voice reminders on her tablet. Now she’s walking every morning and says she feels like herself again. I’m sharing this with my entire family. If you’re reading this and your loved one is on multiple meds - don’t wait. Do it today. It’s not a chore. It’s a gift.
So you want people to make a plan? Fine. But don’t act like this is some revolutionary idea. We’ve had pill organizers since the 80s. The real problem? Doctors don’t listen. Pharmacists are rushed. And no one cares until someone ends up in the ER. This plan is just a Band-Aid on a bullet wound.
Oh sure, let’s all just make little charts and feel good about ourselves while Big Pharma laughs all the way to the bank. Did you know the same companies that sell you the meds also sell the apps and pillboxes? They profit from your confusion. They want you dependent. They want you ‘adherent.’ They don’t want you cured. This whole MAP thing? It’s just another way to make you feel like the problem is you - not the system that charges $500 for a pill that costs $2 to make.
Germany’s got a law for this? That’s cute. In America we have something better - free market competition. If people want a plan, they’ll pay for it. If they don’t, they’ll die. That’s capitalism. No one’s forcing you to take pills. If you forget, you’re just not motivated enough. Maybe you need a motivational speaker, not a pamphlet.
bro i just use my phone alarms and it works fine. why do i need a whole plan? also i think the guy in the article who used sticky notes is kinda a dork.
While the notion of a structured medication action plan may superficially appear to confer tangible benefits regarding therapeutic adherence, a critical examination reveals its inherent epistemological fragility. The assumption that textual or visual cues can supplant the cognitive architecture necessary for long-term compliance is not empirically substantiated. Moreover, the reliance upon care teams presupposes an equitable distribution of medical resources - a condition antithetical to the structural realities of American healthcare. Consequently, the MAP, far from being a panacea, functions as a neoliberal artifact: a performative gesture of patient empowerment that absolves systemic failure of responsibility.
Let me guess - you’re one of those people who thinks a checklist fixes everything. You’re not solving the problem. You’re just decorating the coffin. You think a color-coded chart stops people from hoarding expired meds because they’re scared to throw them out? You think a ‘medication plan’ stops the guy who sells his insulin to pay rent? This isn’t a solution. It’s a distraction. And you’re all just feeling good about yourselves while the system burns.